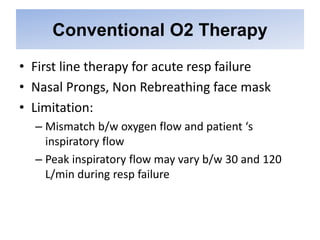
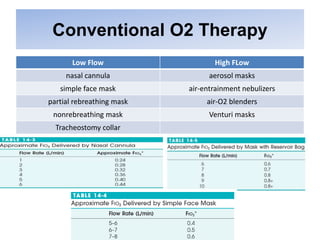
This document discusses different oxygen therapy techniques including conventional oxygen therapy and high flow nasal cannula (HFNC) oxygen therapy. It provides details on:
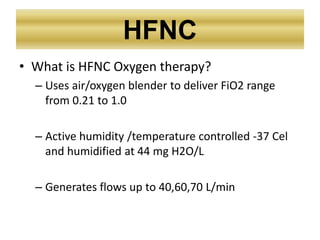
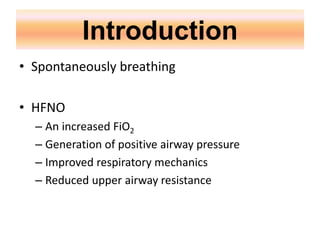
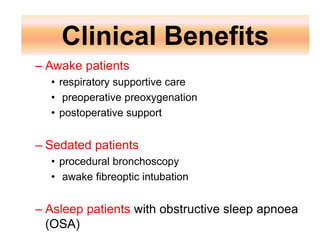
- How HFNC works by using an air/oxygen blender to deliver high flows of humidified oxygen at variable concentrations.
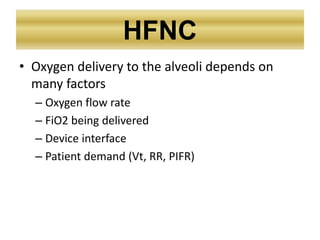
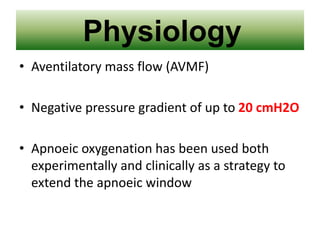
- The physiologic effects of HFNC including improved oxygen delivery to the alveoli and prevention of adverse effects from lack of humidification.
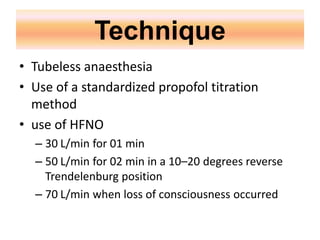
- Techniques called THRIVE and STRIVE-Hi that use HFNC to provide apneic oxygenation and tubeless anesthesia, extending the time available to secure an airway without risk of hypoxemia.