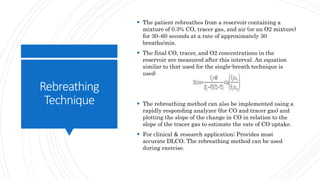
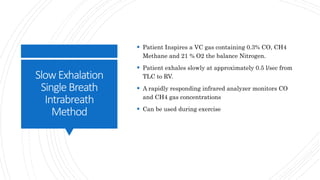
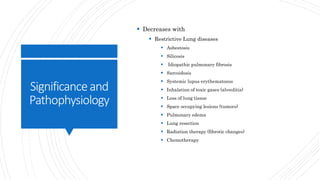
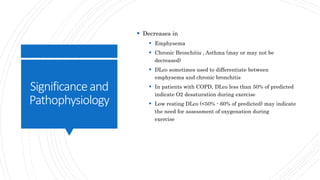
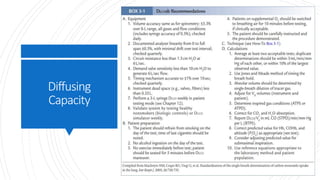
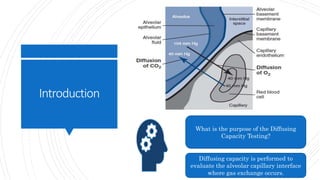
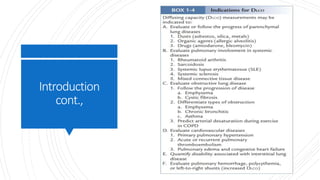
This lecture covers diffusing capacity testing, specifically the single-breath carbon monoxide diffusing capacity (DLCO) test. DLCO measures the transfer of carbon monoxide across the alveolar-capillary membrane and is used to evaluate gas exchange ability. The single-breath method involves rapid inhalation of a test gas mixture containing carbon monoxide to total lung capacity, a 10 second breath hold, and analysis of exhaled gases. DLCO may be reduced in conditions involving decreased alveolar surface area or pulmonary capillary blood volume such as emphysema. Physiologic factors like hemoglobin, carboxyhemoglobin, and pulmonary blood volume also impact DLCO values.

![CARBON
MONOXIDE
DIFFUSING
CAPACITY
DESCRIPTION
DLCO measures the transfer of a diffusion-limited gas
(CO) across the alveolocapillary membranes.
DLCO is reported in milliliters of CO/minute/millimeter
of mercury at 0°C, 760 mm Hg, dry (i.e.,[STPD]).](https://image.slidesharecdn.com/pft4-171autosaved-171120023549/85/Diffusing-Capacity-Tests-6-320.jpg)