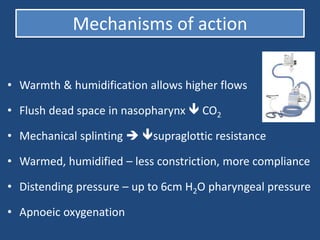
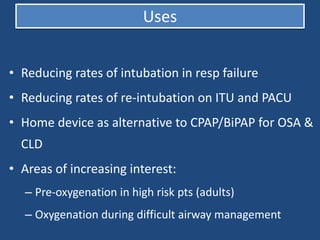
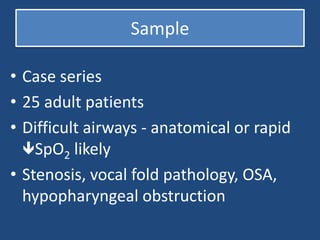
THRIVE is a method using warmed, humidified high flow oxygen via the nose to increase apnea time in patients with difficult airways. It works by flushing carbon dioxide from the nasopharynx, providing mechanical splinting and distention pressure, and allowing apneic oxygenation. A case series of 25 patients with difficult airways found THRIVE increased the median apnea time to 17 minutes without any oxygen saturations dropping below 90%, allowing more time for airway management. While observational and involving expert airway management, the study concludes THRIVE can safely extend the apnea window for difficult airway situations.