This document provides information on non-invasive ventilation (NIV) including:
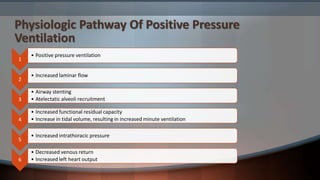
1. The physiologic effects of positive pressure ventilation such as increased laminar flow and alveolar recruitment.
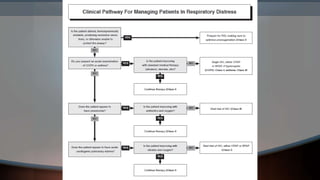
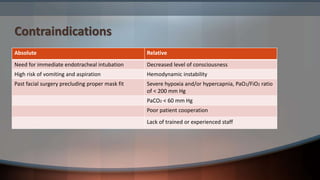
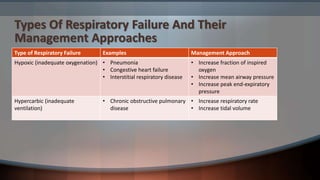
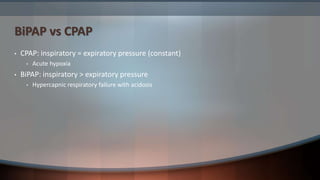
2. Contraindications and types of respiratory failure and their management approaches. BiPAP is used for hypercapnic failure with acidosis while CPAP is used for acute hypoxia.
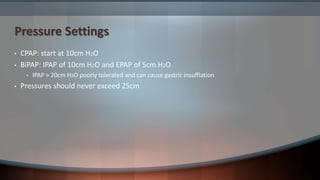
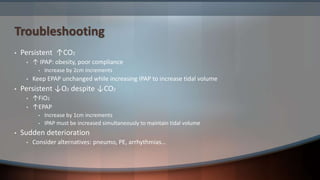
3. Guidelines for setting pressures on CPAP and BiPAP and troubleshooting persistent hypoxia or hypercapnia by adjusting pressures.
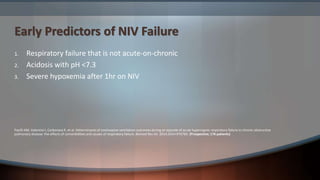
4. Early predictors of NIV failure including a pH <7.3 and lack of acute worsening of chronic respiratory failure.
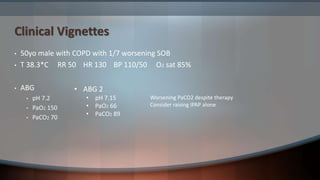
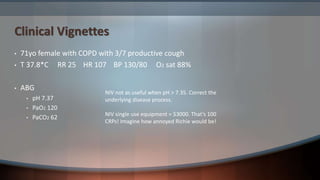
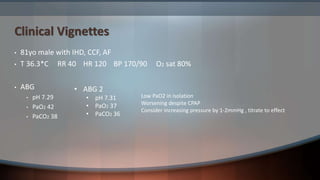
5. Clinical vignettes describing