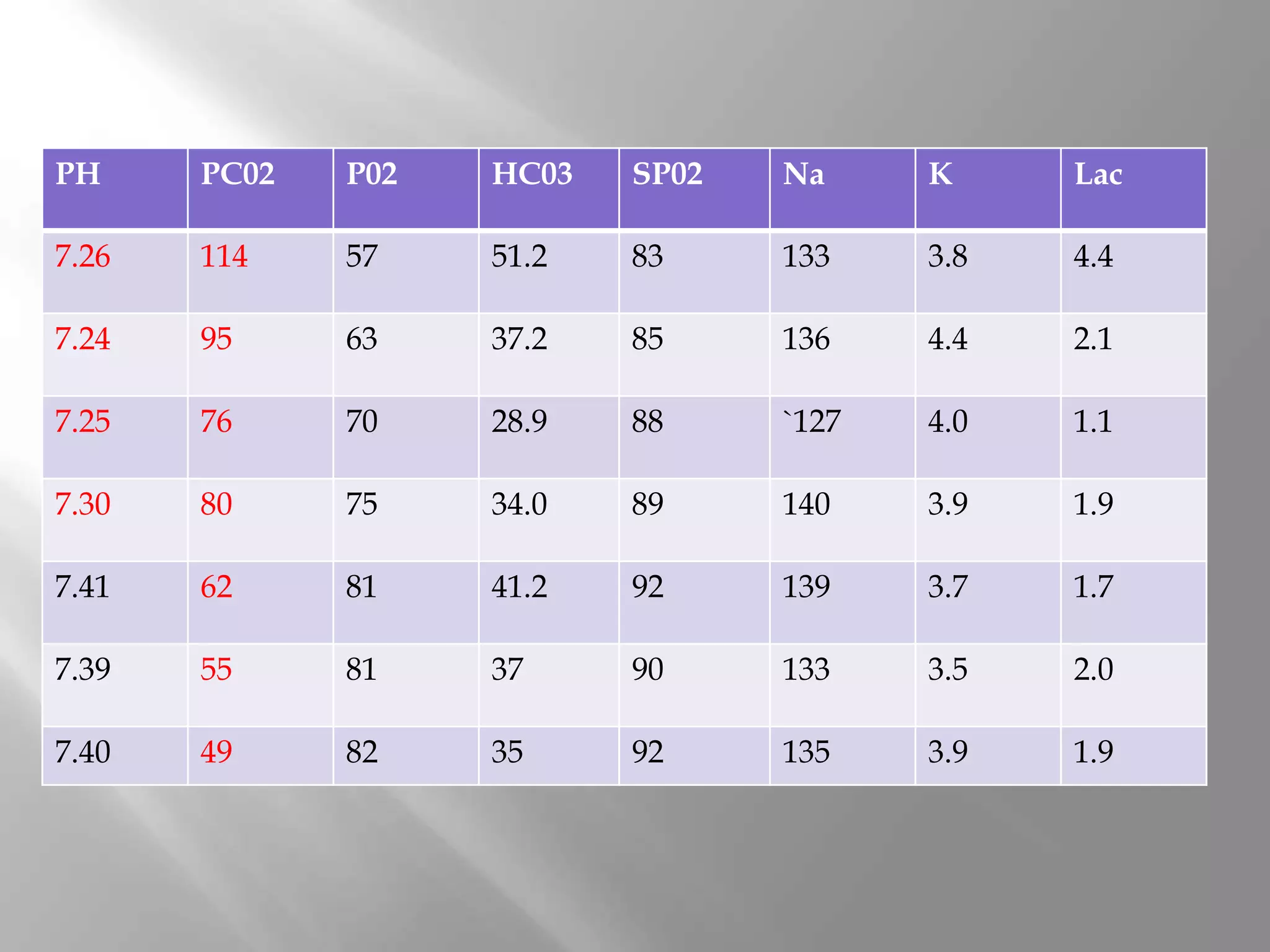
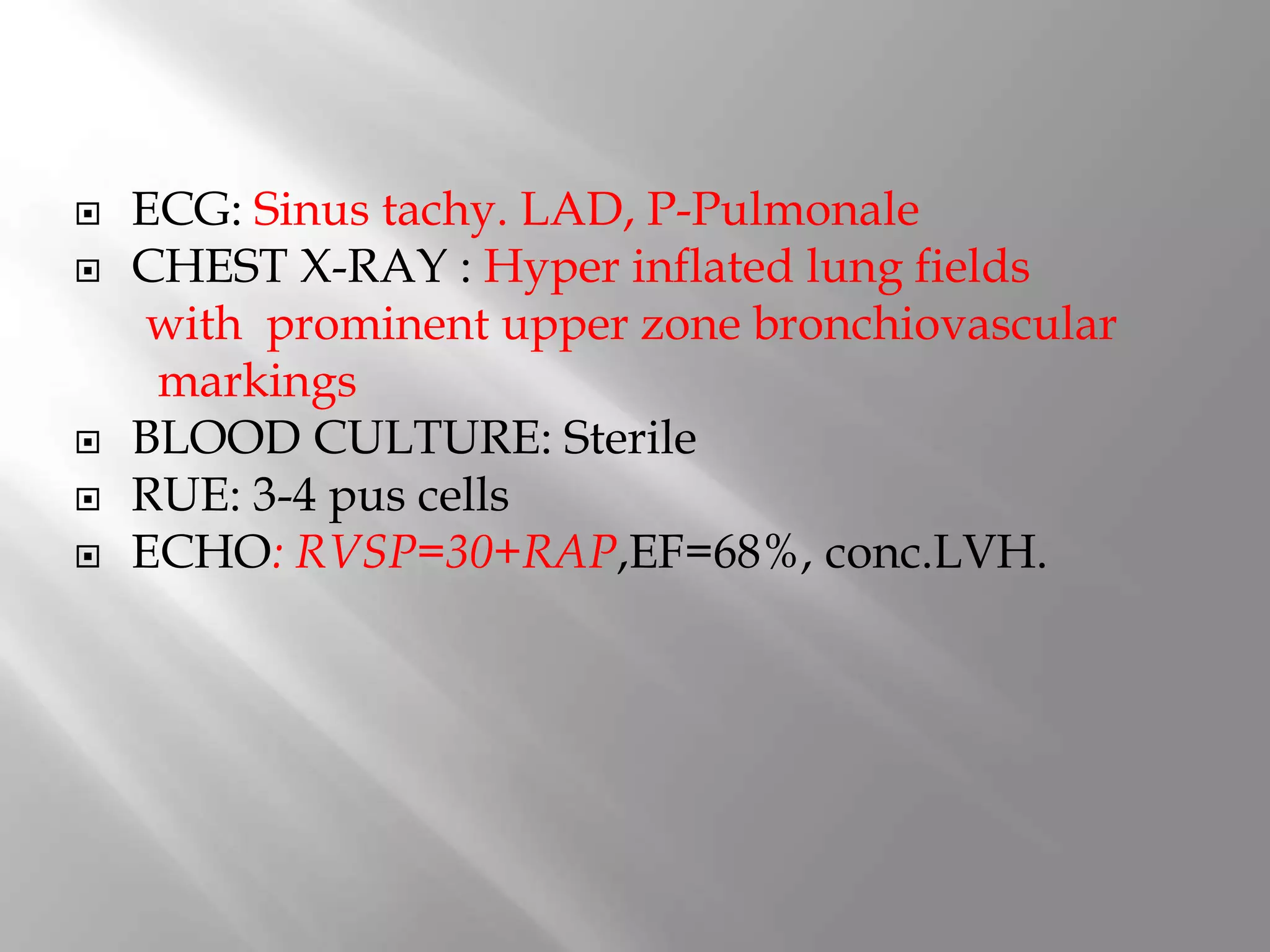
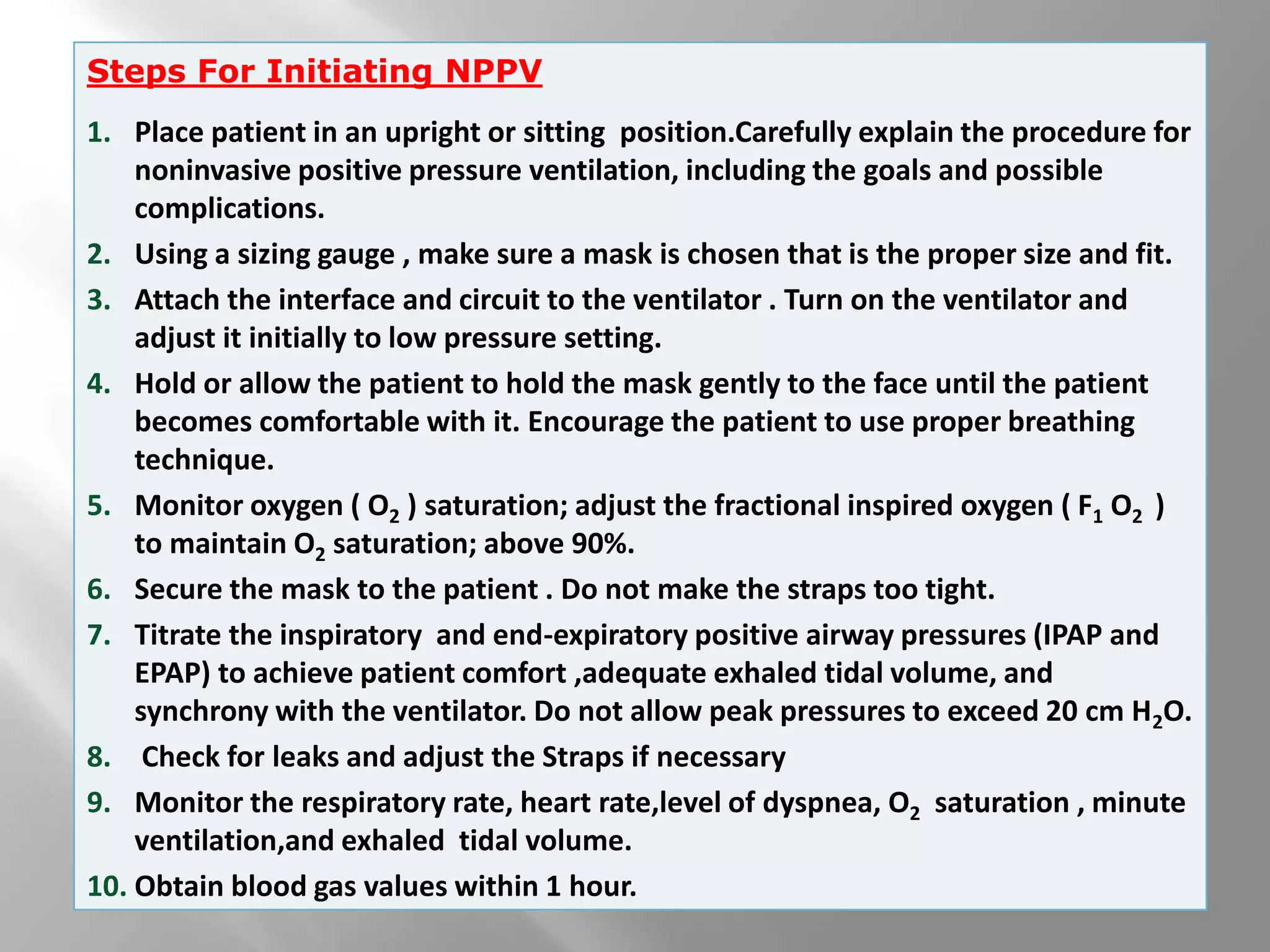
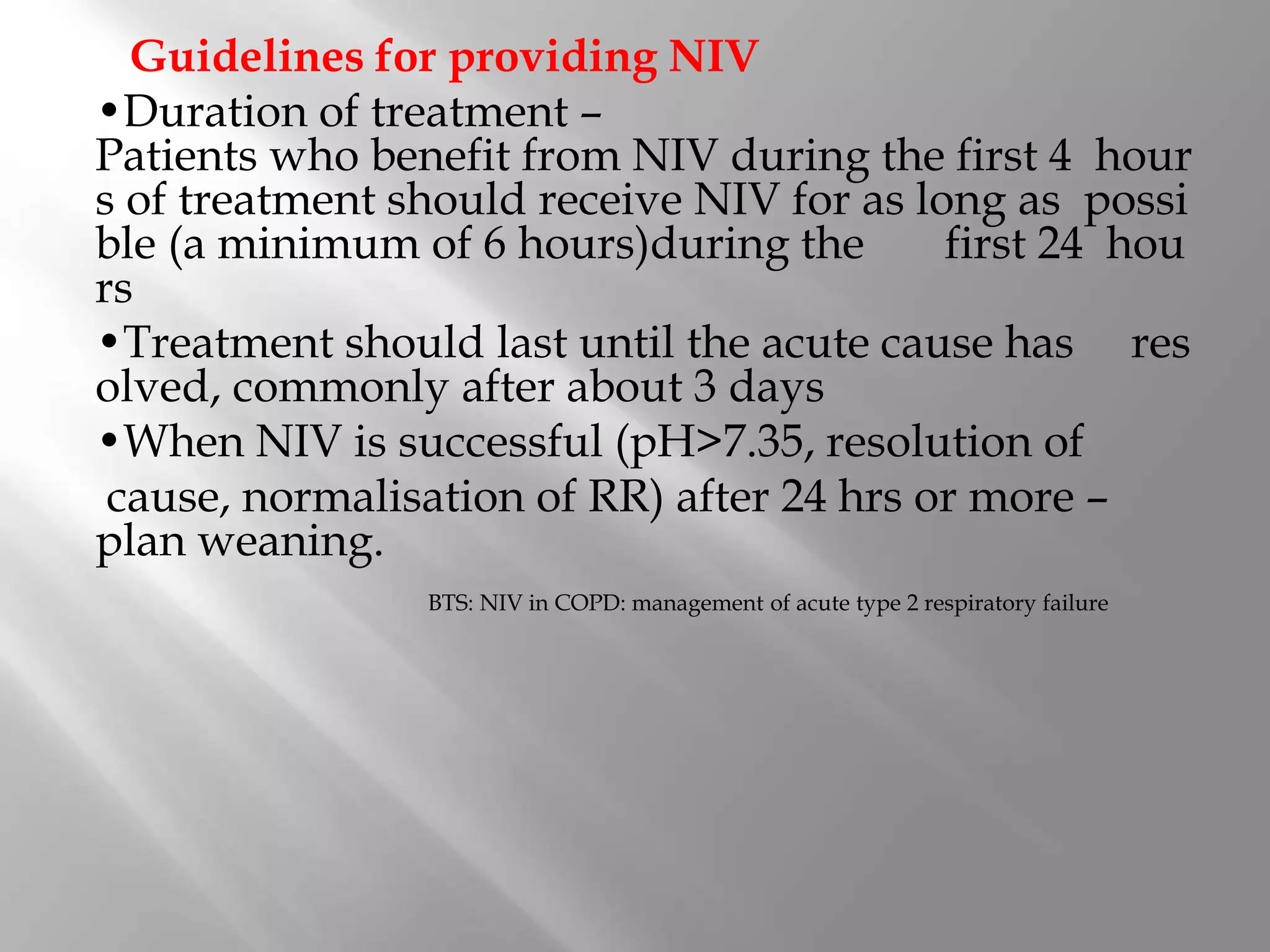
A 62-year-old female with a history of hypertension, diabetes, and COPD presented with worsening cough, expectoration, and breathlessness over the past 3 days. On examination, she was drowsy with tachycardia, tachypnea, and low oxygen saturation. Tests showed respiratory acidosis and congestive cardiac failure. She was started on non-invasive ventilation (NIV) with initial settings of IPAP 10 cm H2O and EPAP 4 cm H2O, which were gradually increased. NIV was given for decreasing durations over 4 days as her condition improved before being discontinued.