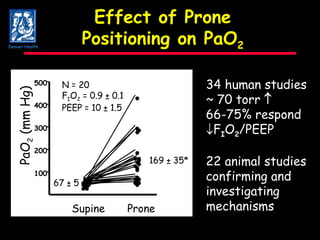
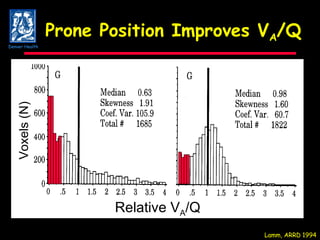
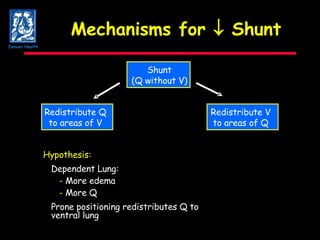
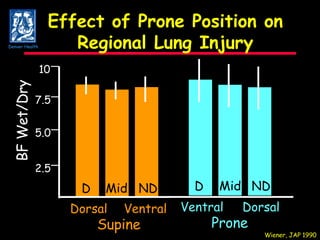
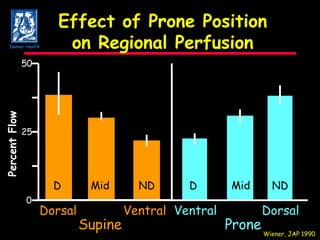
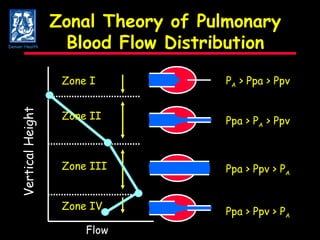
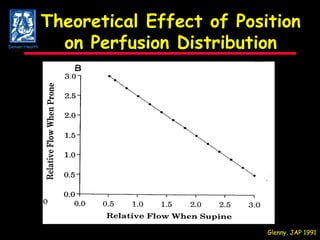
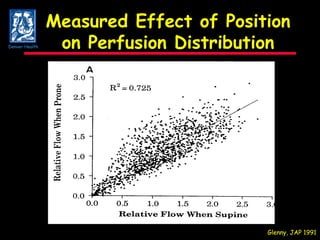
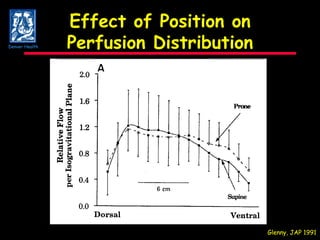
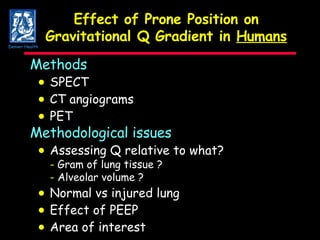
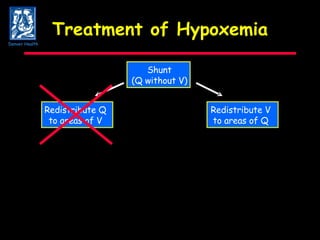
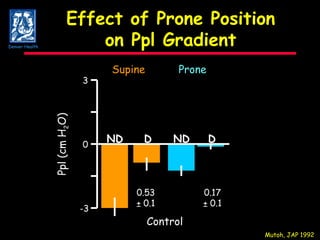
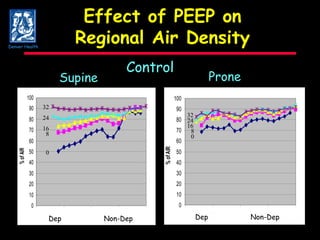
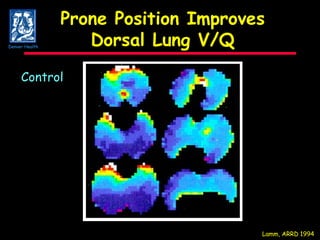
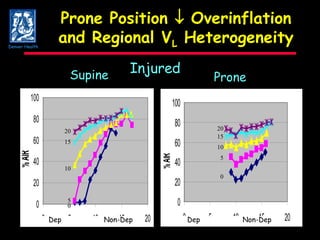
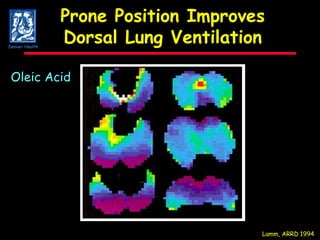
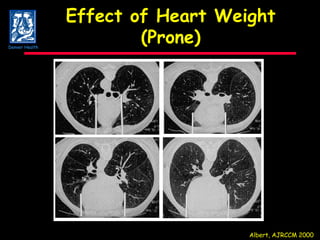
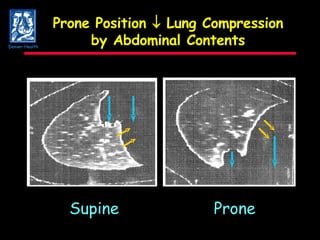
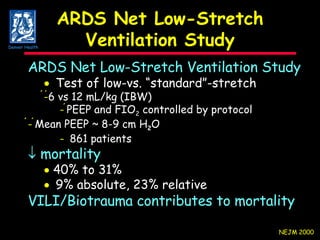
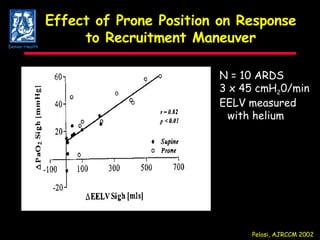
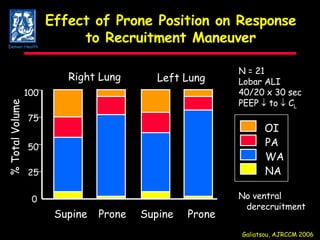
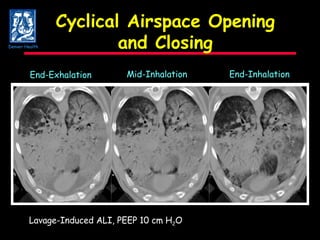
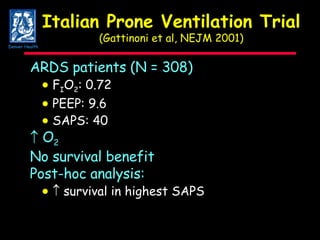
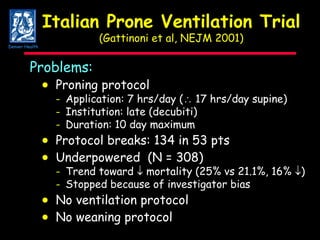
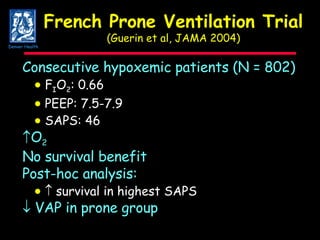
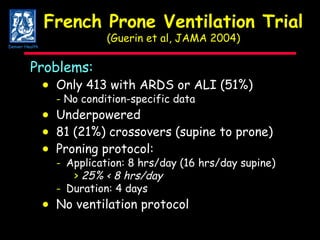
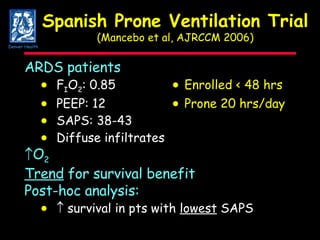
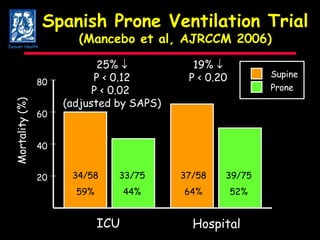
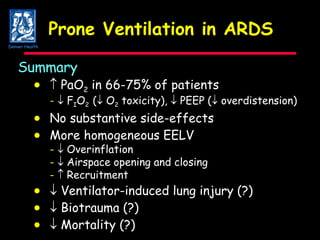
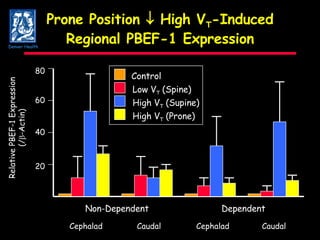
Prone ventilation improves oxygenation in ARDS patients by redistributing ventilation and perfusion away from dependent lung regions. Several clinical trials found no clear survival benefit of prone ventilation overall, but some showed benefits for subgroups with higher illness severity. New research suggests prone positioning may reduce ventilator-induced lung injury by decreasing regional overdistension and making ventilation more homogeneous.