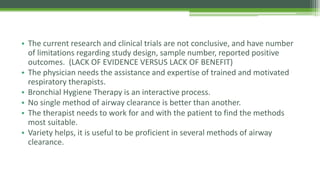
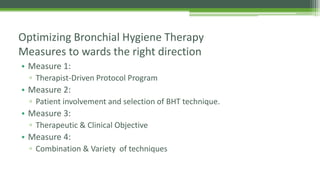
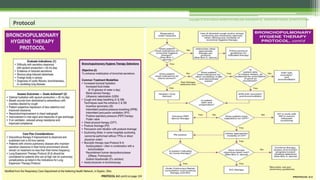
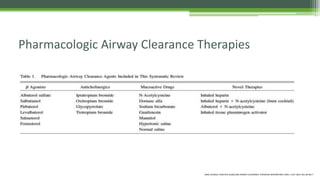
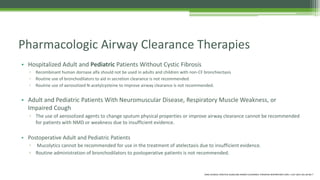
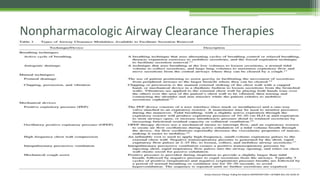
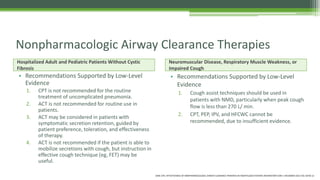
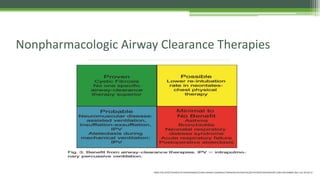
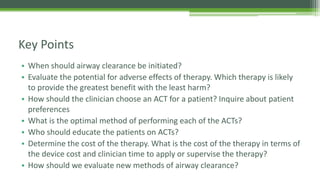
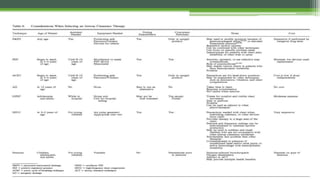
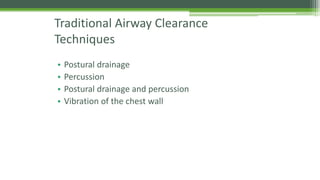
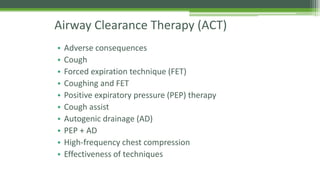
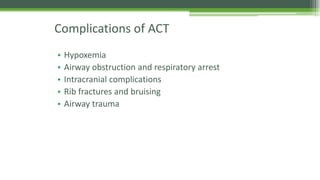
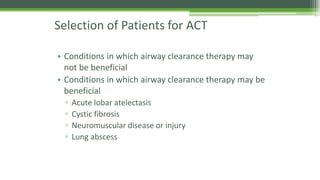
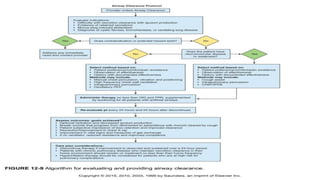
This document provides information about optimizing bronchial hygiene therapy presented by Ahmed Al Gahtani. It discusses various airway clearance therapies including pharmacologic therapies like mucolytics and bronchodilators as well as non-pharmacologic therapies like breathing techniques and mechanical devices. It emphasizes the importance of individualizing treatment, involving patients in selecting techniques, combining different techniques, and evaluating therapies based on clinical objectives and outcomes.