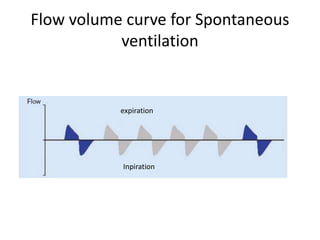
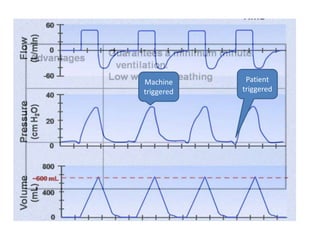
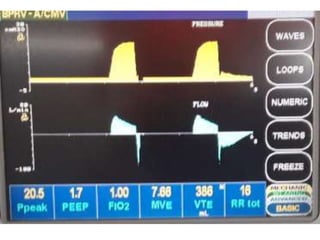
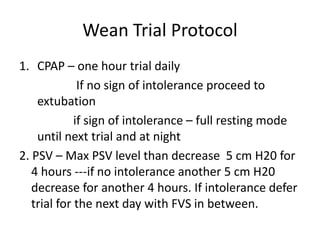
The document discusses basic ventilator management, including the history and types of mechanical ventilation (negative and positive pressure). It outlines indications and exclusion criteria for non-invasive and invasive positive pressure ventilation, as well as guidelines for initial ventilator settings and monitoring. Additionally, it covers weaning procedures and potential complications associated with mechanical ventilation.