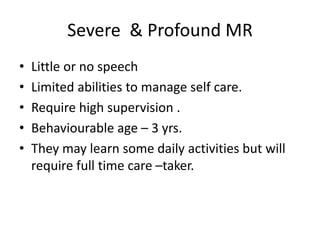
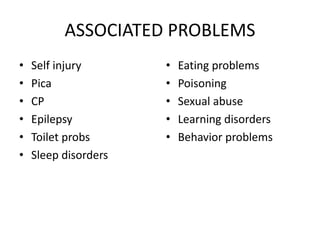
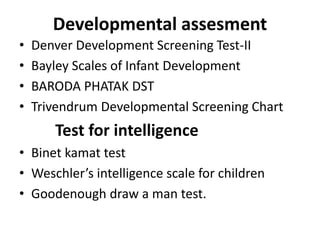
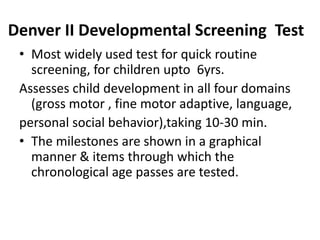
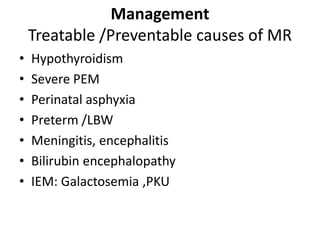
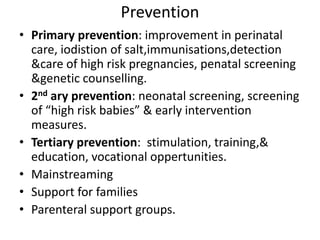
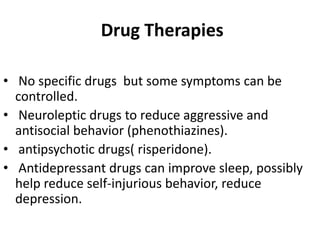
This document provides information on mental retardation (MR), including its definition, prevalence, grades, signs and symptoms, developmental assessment tests, and management approach. MR affects about 1-3% of the population and is characterized by below-average intellectual functioning and adaptive deficits. It is diagnosed based on clinical features and assessment of intellectual functioning using IQ tests. Management focuses on identifying treatable causes, providing early intervention, education/training, and supporting independent living.