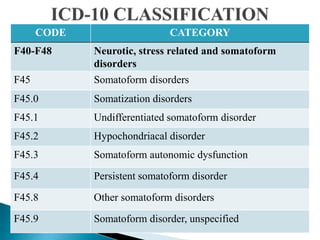
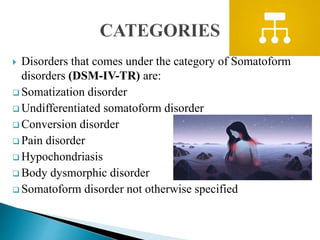
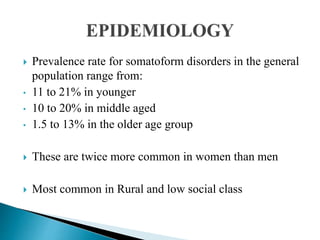
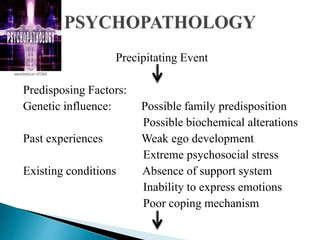
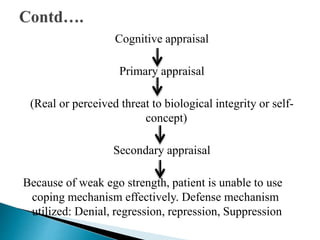
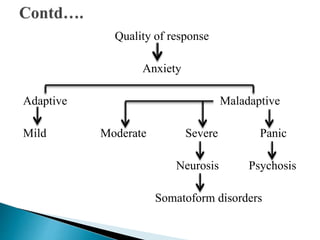
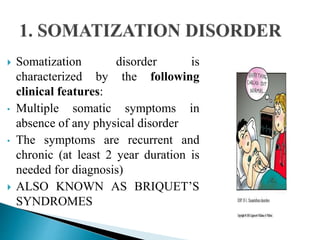
This document discusses somatoform disorders. It begins by defining somatoform disorders as mental illnesses characterized by physical symptoms that cannot be fully explained medically and cause impairment. Key points include: somatoform disorders involve the presentation of physical complaints due to psychological factors; they are characterized by multiple somatic complaints and persistent healthcare seeking despite reassurance; and common types include somatization disorder, conversion disorder, and hypochondriasis. Treatment involves identifying and addressing the underlying psychological causes through cognitive behavioral therapy and other approaches.