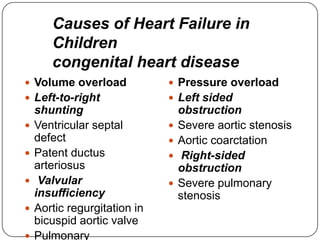
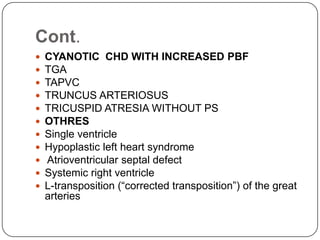
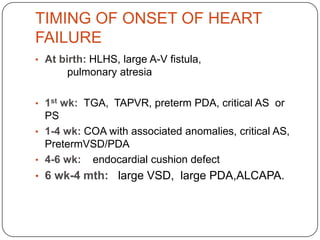
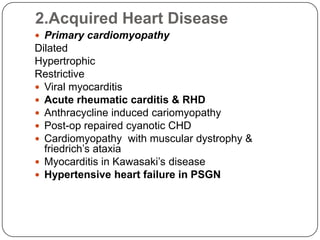
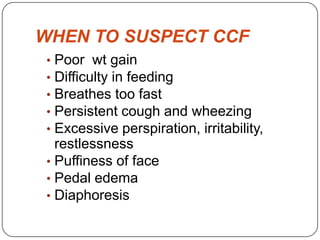
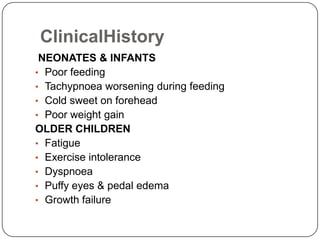
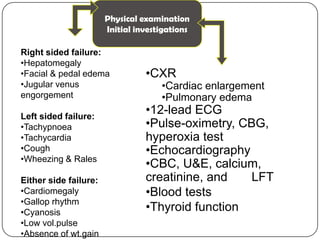
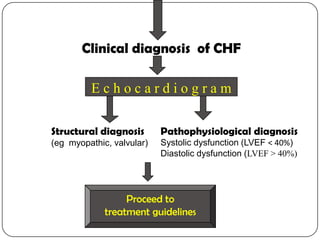
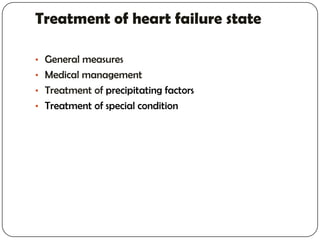
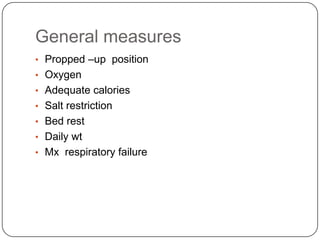
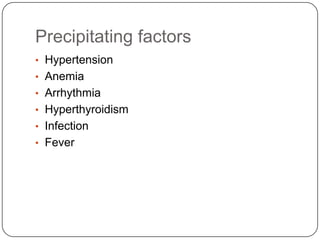
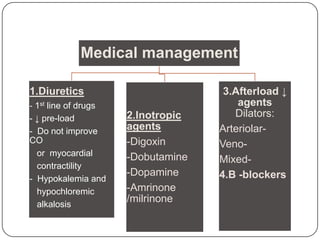
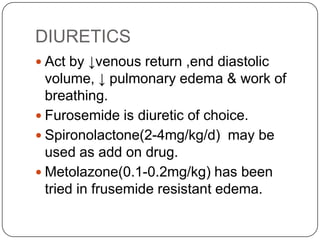
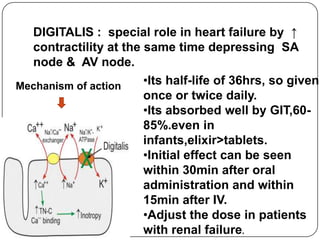
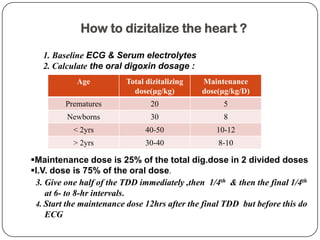
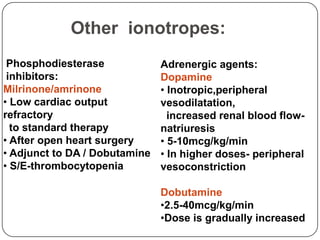
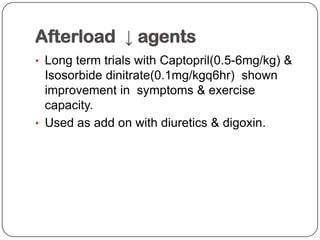
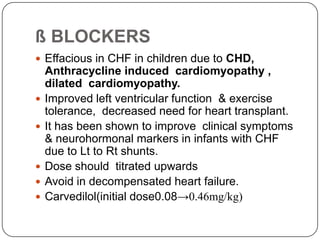
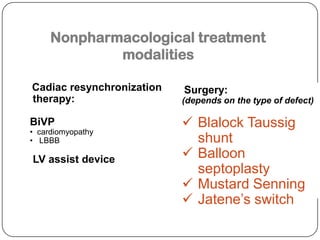
This document discusses heart failure in pediatrics. It defines heart failure as the heart's inability to pump enough blood to meet the body's needs. The main causes in children are congenital heart defects and acquired conditions like cardiomyopathy. Common congenital defects that can lead to heart failure include single ventricle, hypoplastic left heart syndrome, and atrioventricular septal defects. Symptoms depend on the age of onset and include poor feeding, fast breathing, cough, and failure to gain weight. Evaluation involves history, exam, echocardiogram, and blood tests. Treatment consists of diuretics, digoxin, and other inotropes to improve cardiac function, along with addressing any precipitating