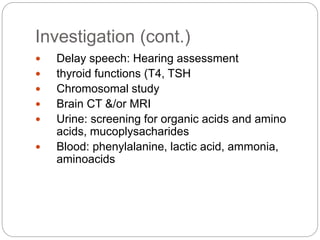
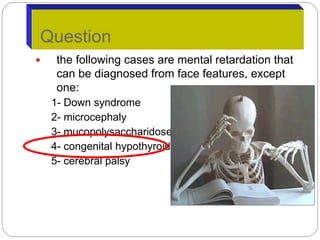
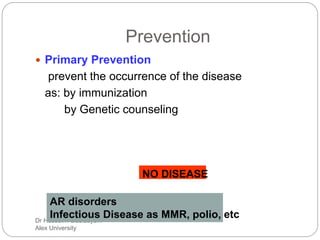
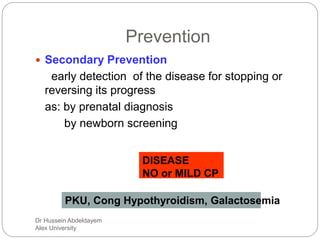
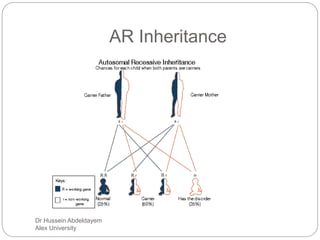
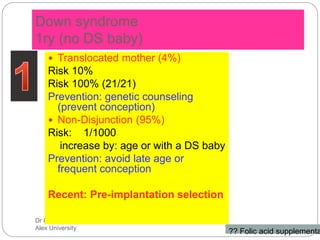
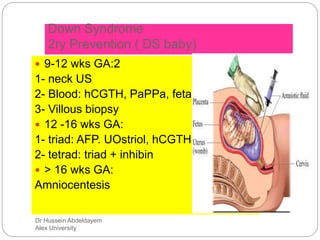
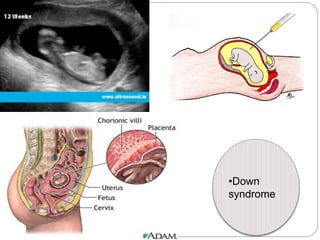
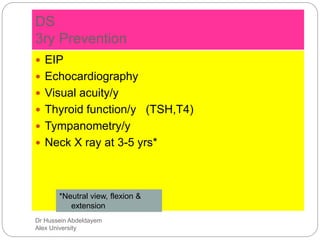
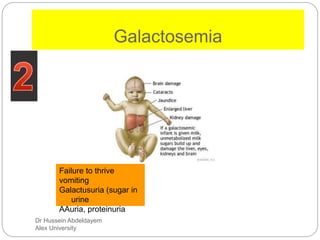
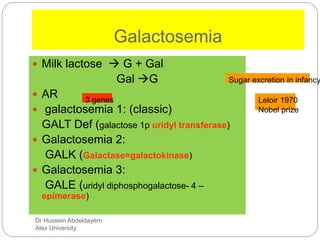
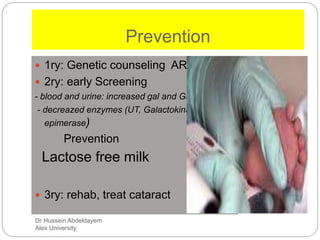
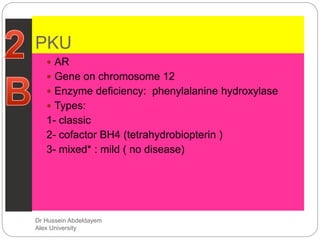
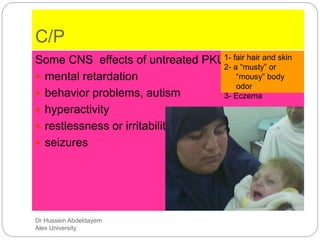
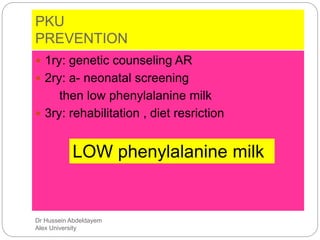
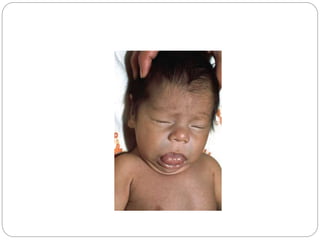
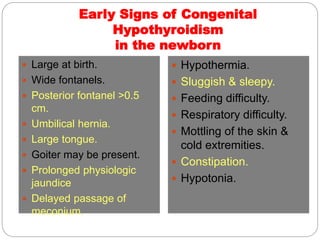
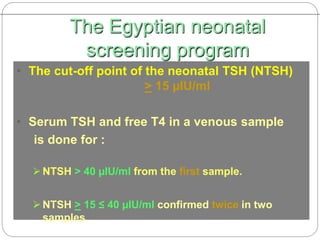
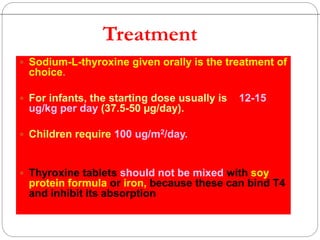
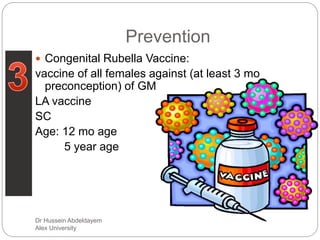
Primary prevention methods can help reduce the occurrence of mental retardation from certain conditions. Early screening through newborn screening can help detect treatable causes like phenylketonuria (PKU), galactosemia, and congenital hypothyroidism to prevent or reduce intellectual disability. Maintaining treatment protocols through dietary or medical management in PKU, galactosemia, maternal PKU, and congenital hypothyroidism is important for tertiary prevention. Genetic counseling can aid primary prevention for conditions with a genetic basis like Down syndrome, galactosemia, and PKU.