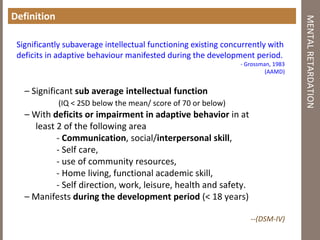
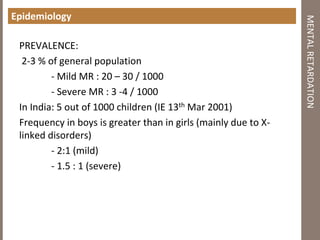
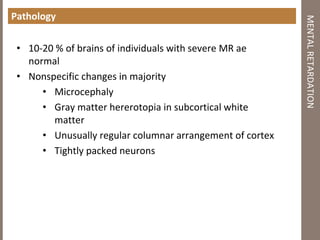
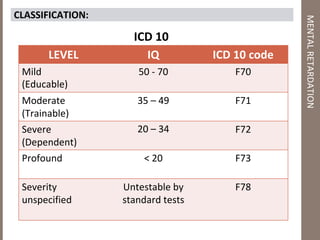
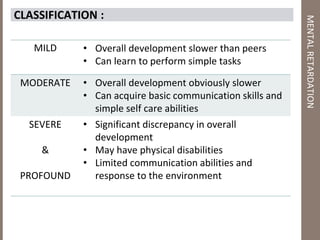
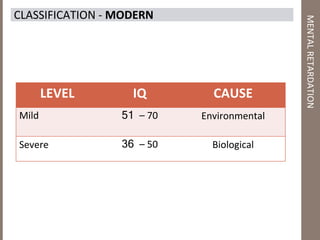
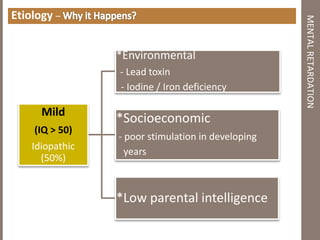
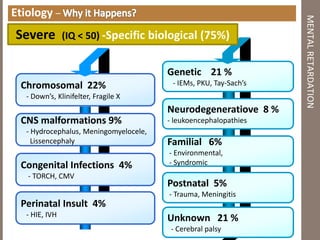
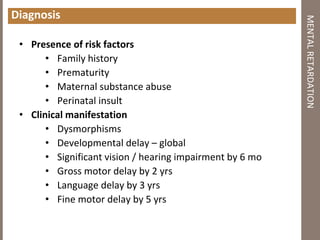
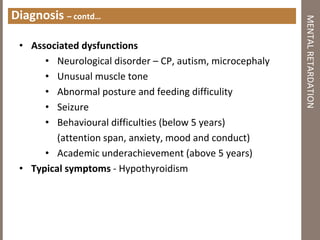
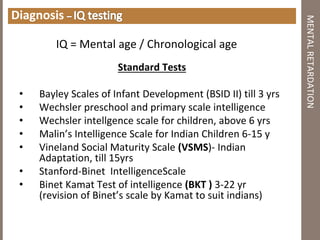
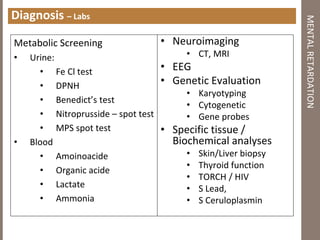
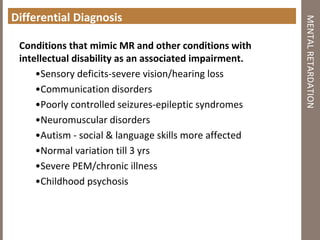
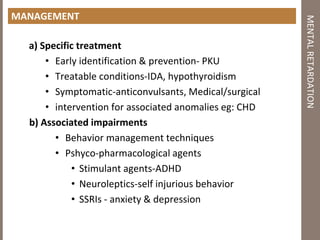
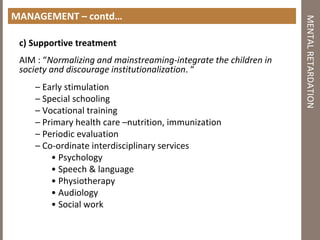
Mental retardation is defined as significantly subaverage intellectual functioning existing concurrently with deficits in adaptive behavior manifested during the development period. It affects 2-3% of the general population and is classified as mild, moderate, severe or profound based on IQ scores. The causes include genetic and chromosomal abnormalities, environmental factors, prenatal and perinatal insults. Management involves early identification, treatment of associated conditions, supportive therapies, special education, vocational training and parental counseling.