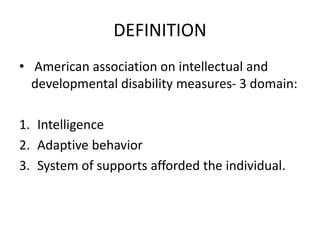
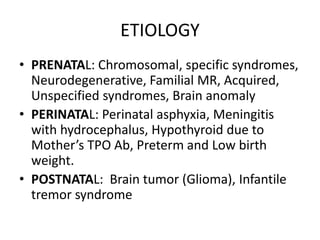
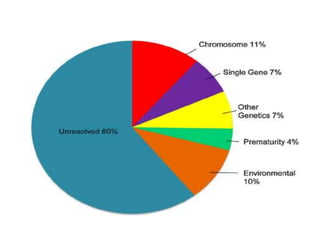
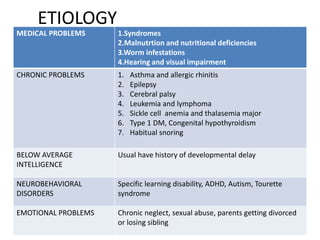
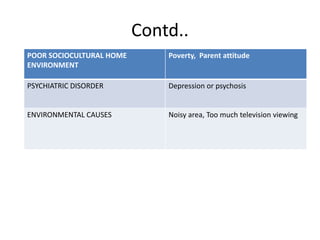
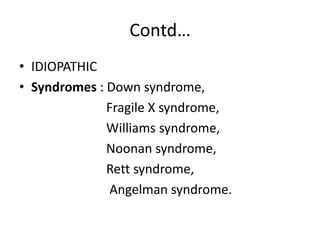
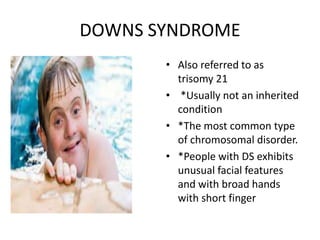
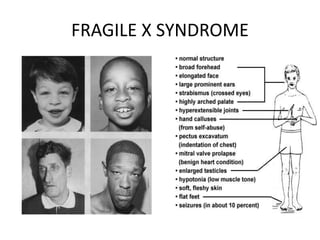
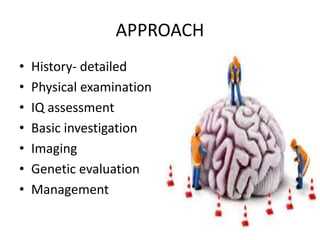
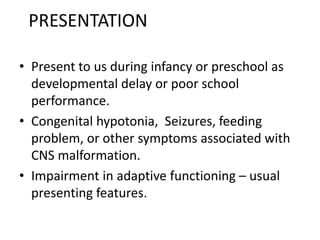
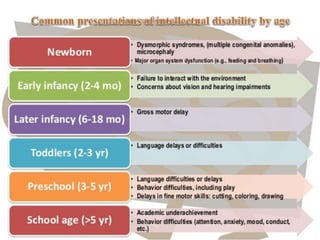
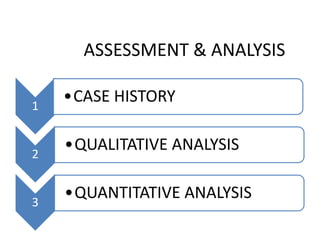
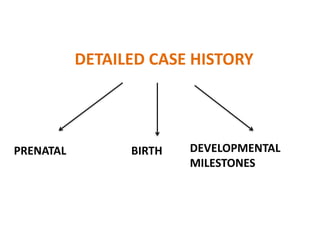
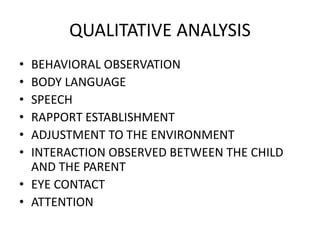
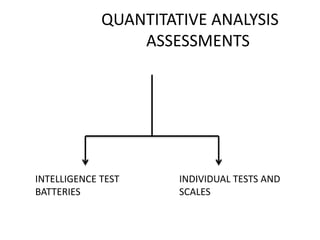
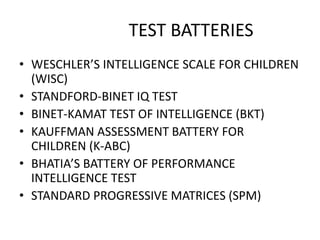
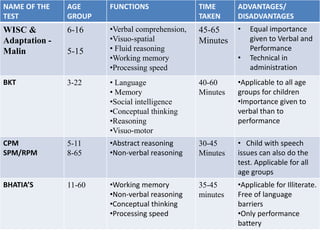
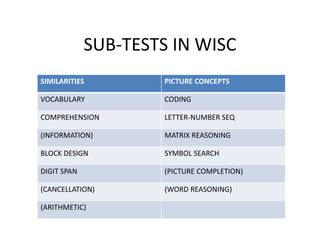
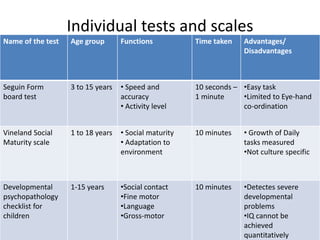
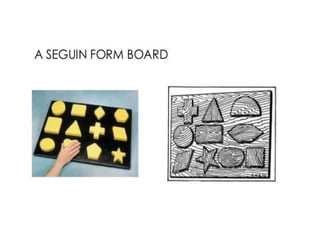
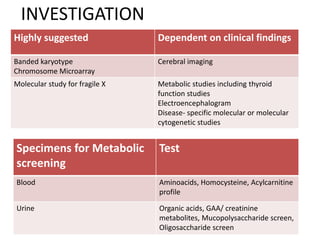
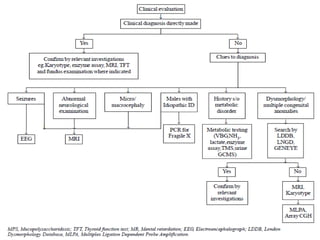
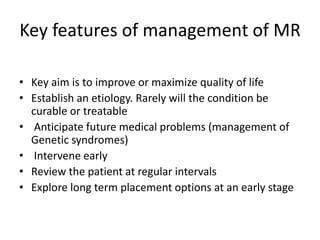
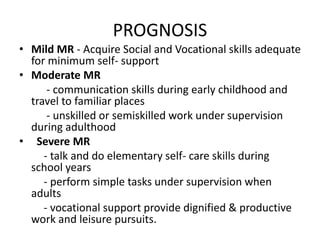
This document provides an overview of intellectual disability (ID). It begins with definitions and causes of ID including prenatal, perinatal, and postnatal factors. Specific genetic syndromes like Down syndrome and Fragile X syndrome are discussed. The approach involves a detailed history, physical exam, IQ assessment using tests like the WISC, and basic investigations. Management aims to improve quality of life through treating medical conditions, nutrition, education/therapy, and supportive services. Prognosis depends on severity of ID. Prevention focuses on identifying issues early and addressing factors like nutrition and healthcare access.
![INTRODUCTION
• Problem encountered in almost all clinical
setting
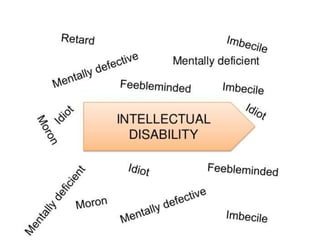
• Other terms- Mental retardation, General
learning disorder and Intellectual impairment.
• 20% children scholastically backward.[Indian J
Pediatr;72(11) : 961-967]
• Occurs in 2-3% of the general
population[INDIAN PAEDIATRICS]](https://image.slidesharecdn.com/approachtointellectualdisability-170525124445/85/Approach-to-intellectual-disability-3-320.jpg)