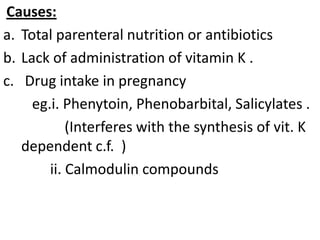
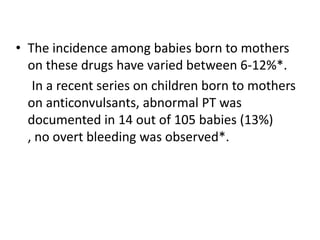
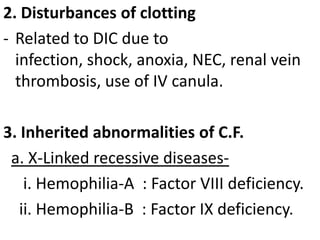
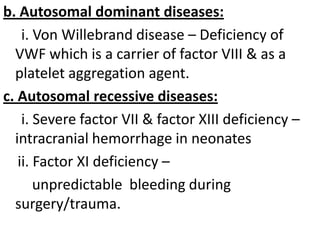
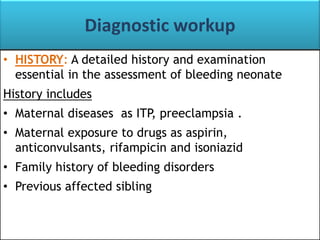
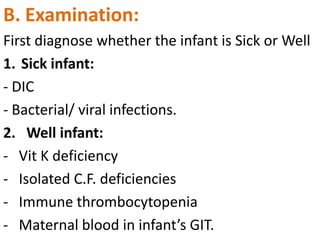
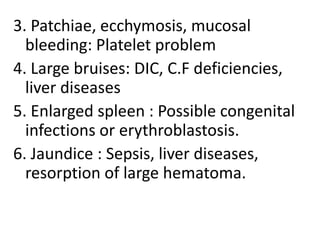
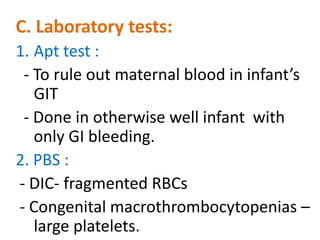
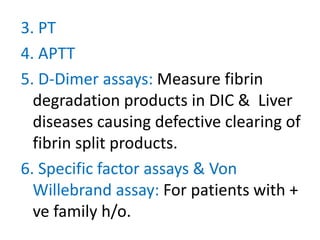
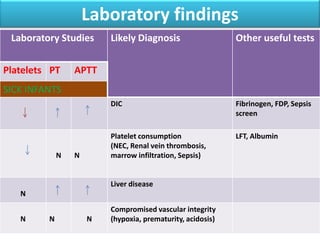
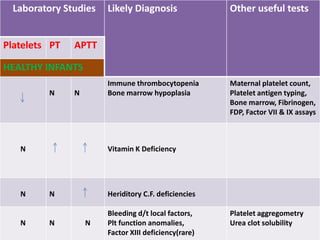
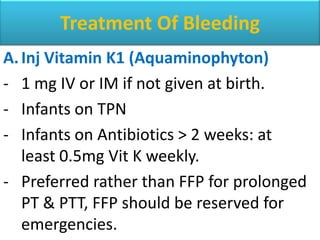
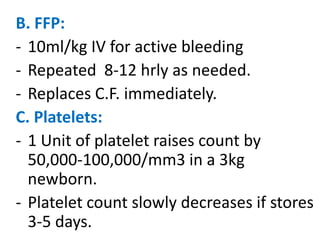
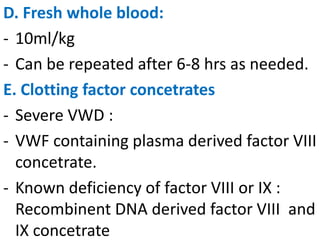
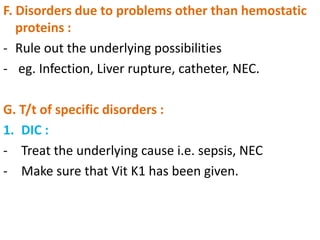
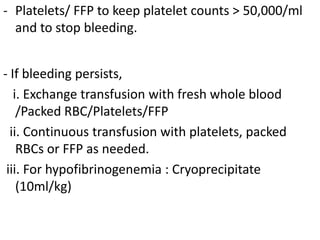
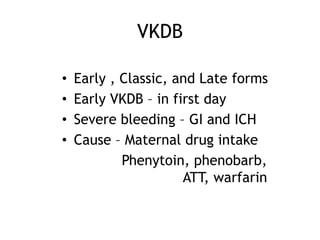
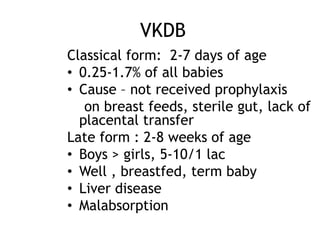
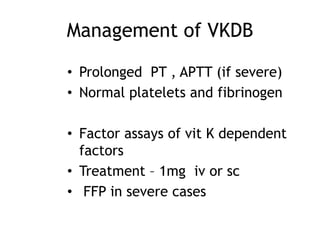
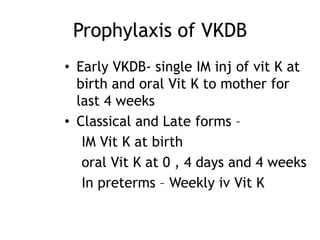
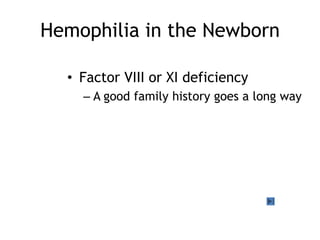
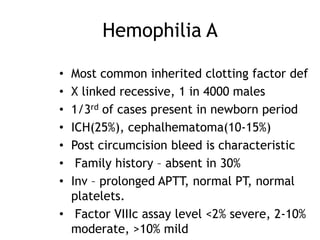
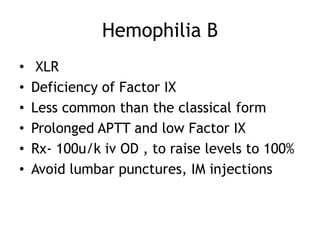
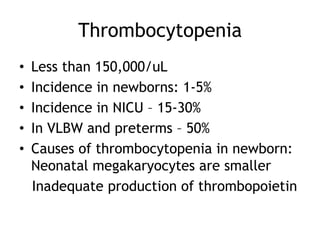
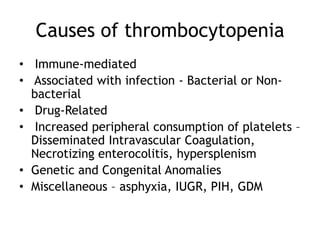
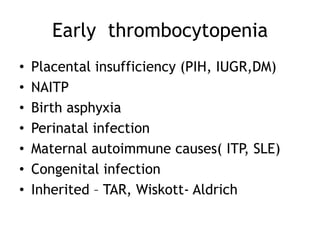
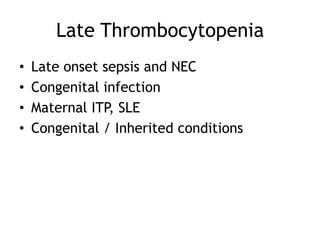
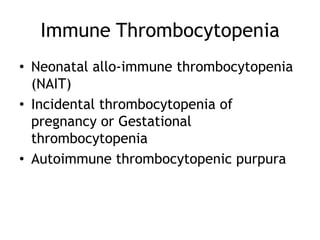
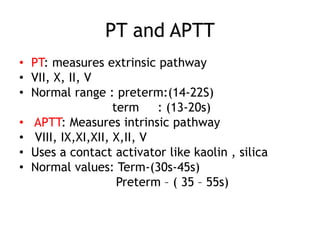
This document summarizes bleeding in neonates. Neonates are susceptible to bleeding due to immature coagulation systems and deficiency of coagulation factors. Bleeding may present as oozing from umbilical stumps or bruising. Etiologies include deficiency of vitamin K dependent coagulation factors, platelet problems, and vascular abnormalities. Diagnostic workup includes history, exam, PT, APTT, and factor assays. Treatment involves vitamin K, fresh frozen plasma, platelets, or specific factor replacements depending on the underlying cause.