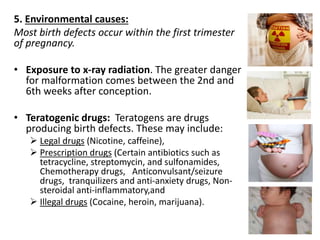
The document discusses the evolving understanding of disability and defines it as the interaction between impairments and various barriers that hinder full participation in society. It details the historical context, current definitions, causes, categories, and rights of individuals with disabilities, particularly focusing on children. The document emphasizes the importance of early childhood intervention, community-based rehabilitation, and multi-sectoral strategies to support the development and inclusion of people with disabilities.