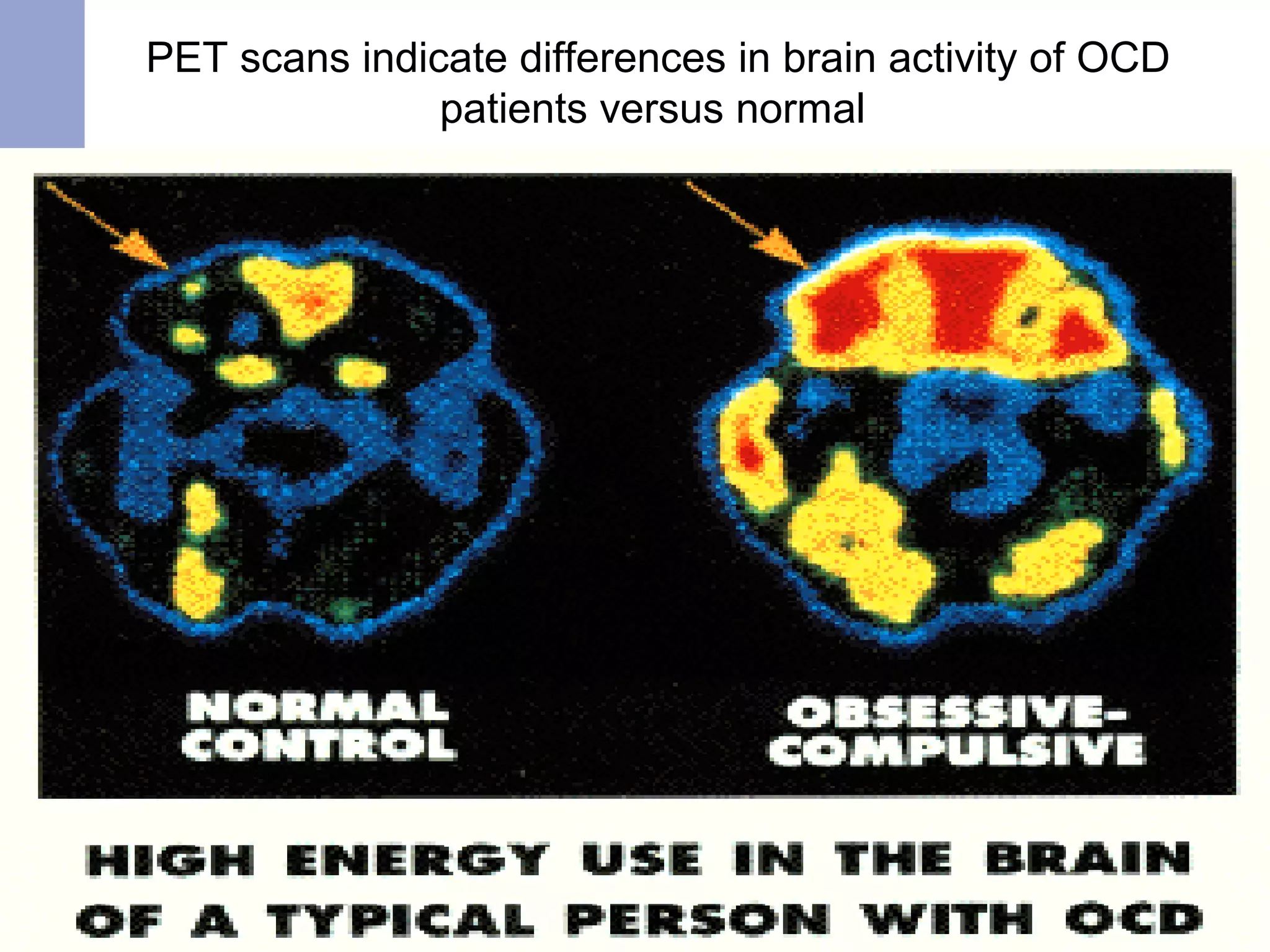
OCD is an anxiety disorder characterized by recurrent obsessions and/or compulsions. It affects approximately 3% of the population worldwide and typically emerges between ages 20-24. While the exact cause is unknown, biological factors like abnormalities in brain circuits and serotonin levels are implicated. Treatment involves cognitive-behavioral therapy such as exposure response prevention and medication like SSRIs. Nursing management focuses on assessing coping abilities, role functioning, and providing psychoeducation on relationships between anxiety, thoughts, and behaviors.