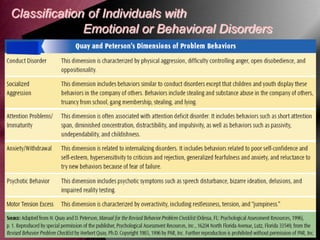
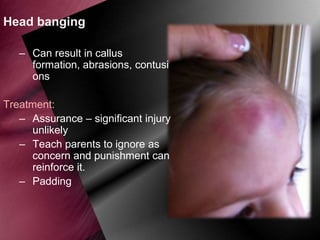
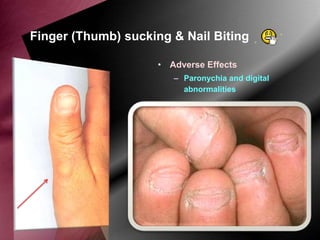
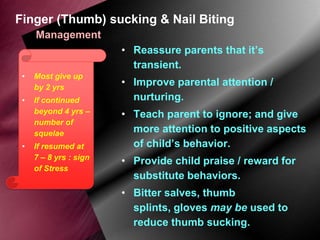
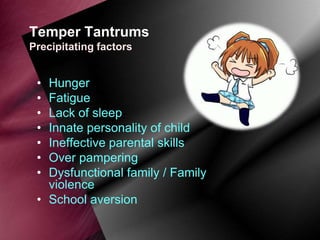
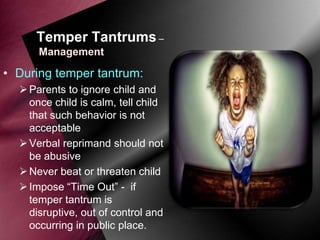
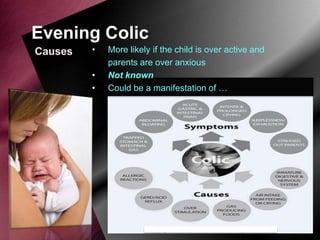
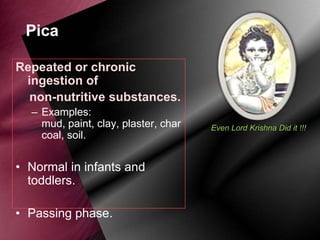
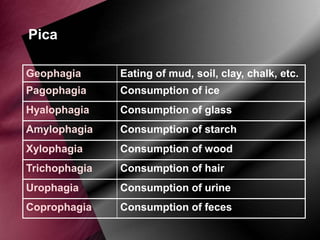
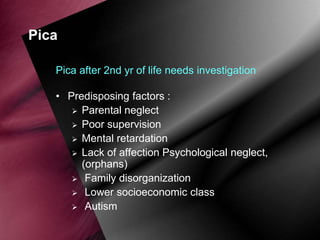
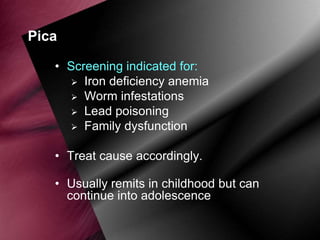
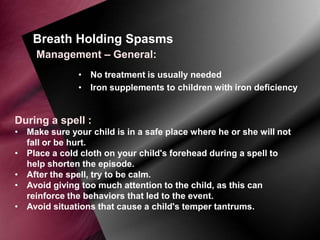
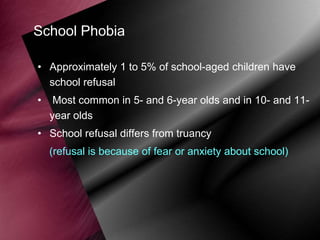
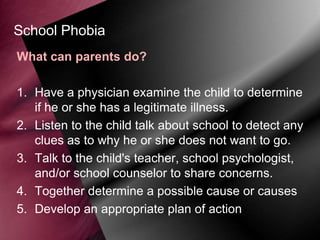
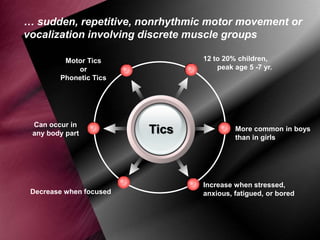
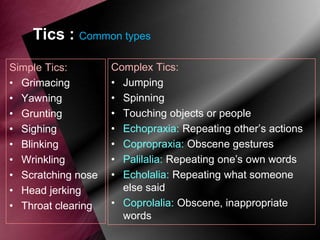
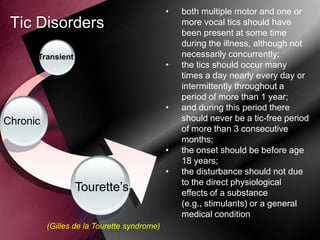
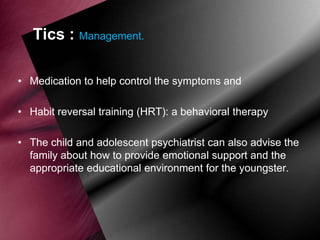
A behaviour disorder in a child is defined as behaviour that is noticeably different from what is expected based on the child's environment and community. Behaviour can be affected by factors such as heredity, environment, learning, and conditioning. Behaviour disorders are categorized into habit disorders like thumb sucking and nail biting, emotional disorders like temper tantrums, eating disorders like pica, and others. The document provides details on the causes, characteristics, and management of various behavioural disorders seen in children such as head banging, nail biting, temper tantrums, colic, pica, breath holding spells, school phobia, stuttering, and tics.