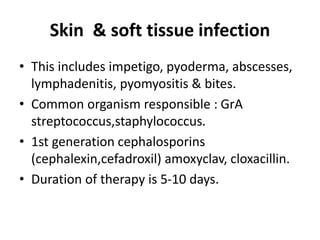
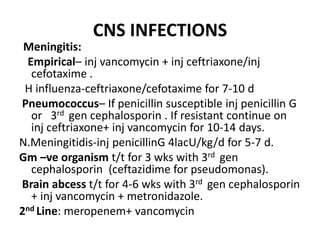
This document provides guidelines for rational antibiotic therapy. It discusses the importance of rational antibiotic use to better care for patients, combat antimicrobial resistance, and reduce costs. It outlines strategies for choosing the appropriate antibiotic based on diagnosis, likely pathogens, sensitivity patterns, and patient factors. Specific antibiotic recommendations are provided for common bacterial infections affecting various body systems like skin, ENT, respiratory, GI, urinary, CNS, and cardiovascular. It also discusses approaches for antibiotic prophylaxis and strategies to prevent antibiotic resistance.