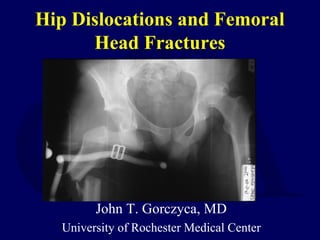
This document provides information on hip dislocations and femoral head fractures. It begins with an introduction noting that hip dislocations caused by significant force are associated with other fractures and damage to the vascular supply of the femoral head, resulting in a high chance of complications. It then discusses anatomy, mechanisms of injury, evaluation, classification, clinical management including emergent treatment and reduction, and indications for operative versus nonoperative treatment. The key points are that hip dislocations