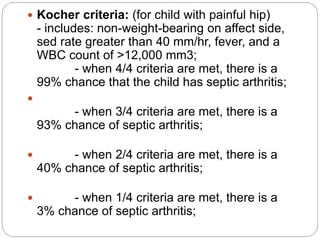
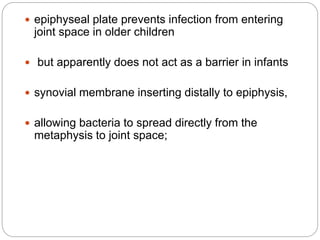
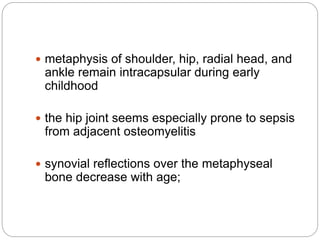
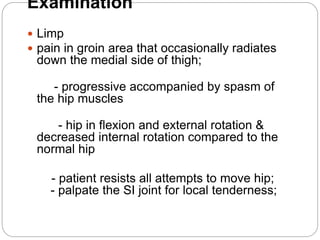
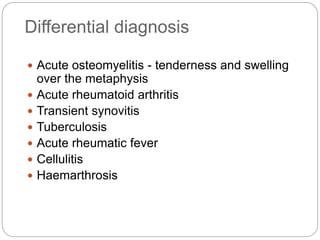
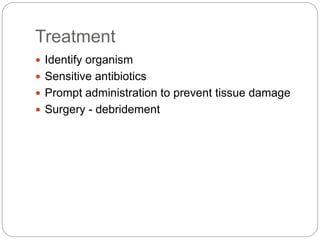
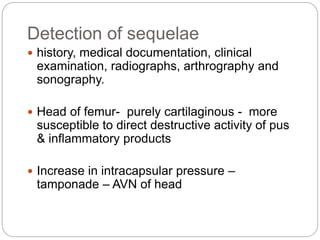
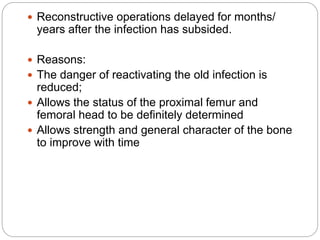
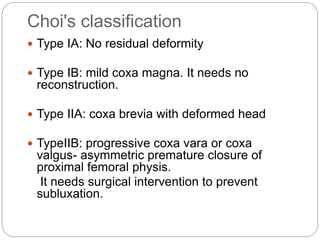
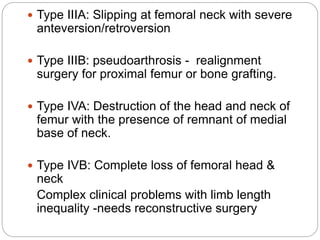
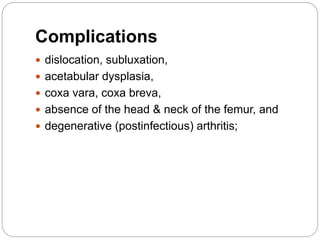
This document discusses septic arthritis of the hip in children. It defines septic arthritis and notes that the hip is the most commonly infected joint in children. Early diagnosis and treatment is important to prevent joint damage. Signs include limping, groin pain, and limited hip movement. Treatment involves identifying the organism, administering sensitive antibiotics, and potentially surgery. Long term sequelae can include joint deformities, leg length discrepancies, and arthritis. Various classification systems and treatment approaches are presented. Prevention of septic arthritis through early diagnosis and management is emphasized.