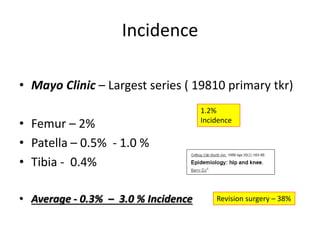
1. Periprosthetic fractures are fractures that occur near a joint replacement prosthesis. They can occur in the femur, patella, or tibia.
2. Risk factors include increasing age, female sex, osteoporosis, revision arthroplasty, rheumatoid arthritis, steroid use, and neurological diseases.
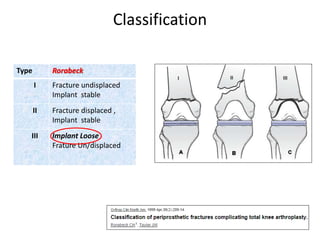
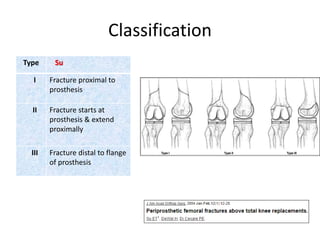
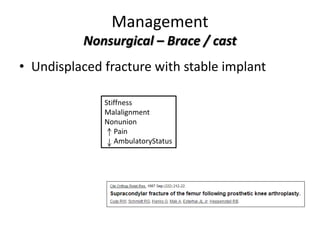
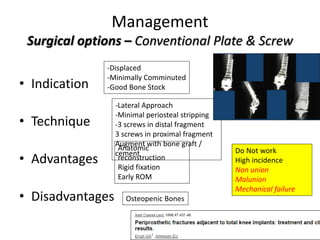
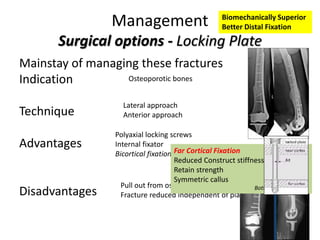
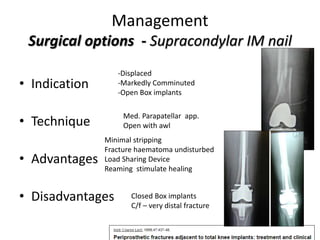
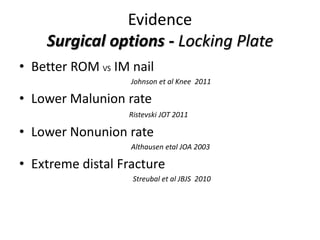
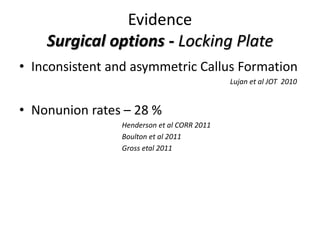
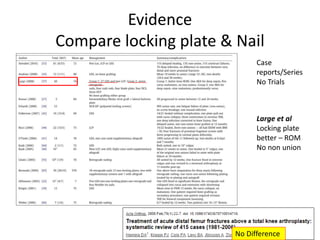
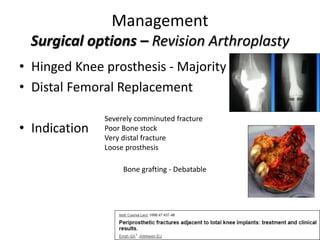
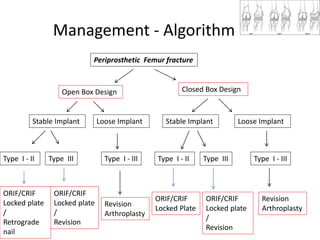
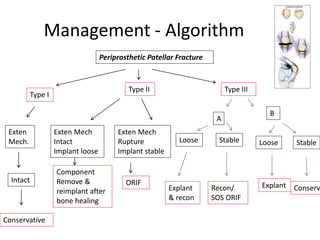
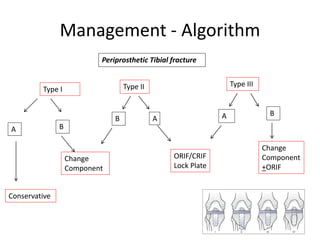
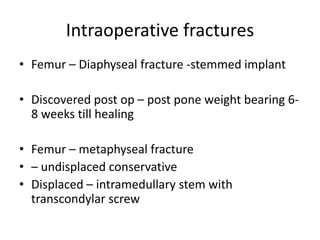
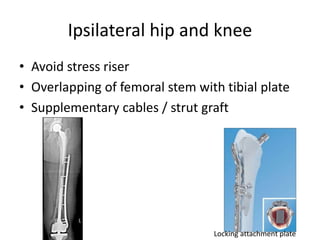
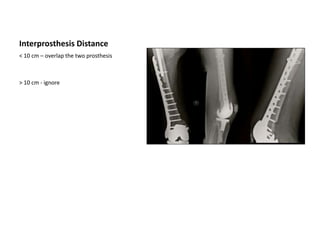
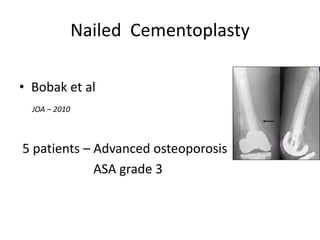
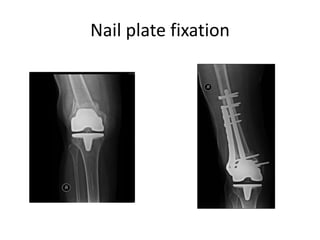
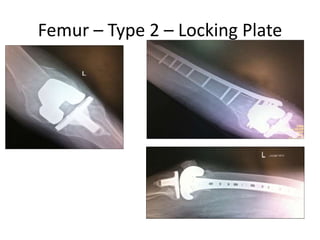
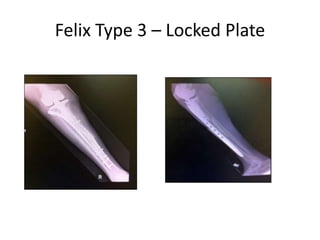
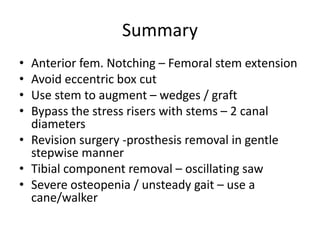
3. Surgical treatment depends on the fracture classification and stability of the prosthesis. Options include open reduction internal fixation with a locking plate, intramedullary nailing, or revision arthroplasty.