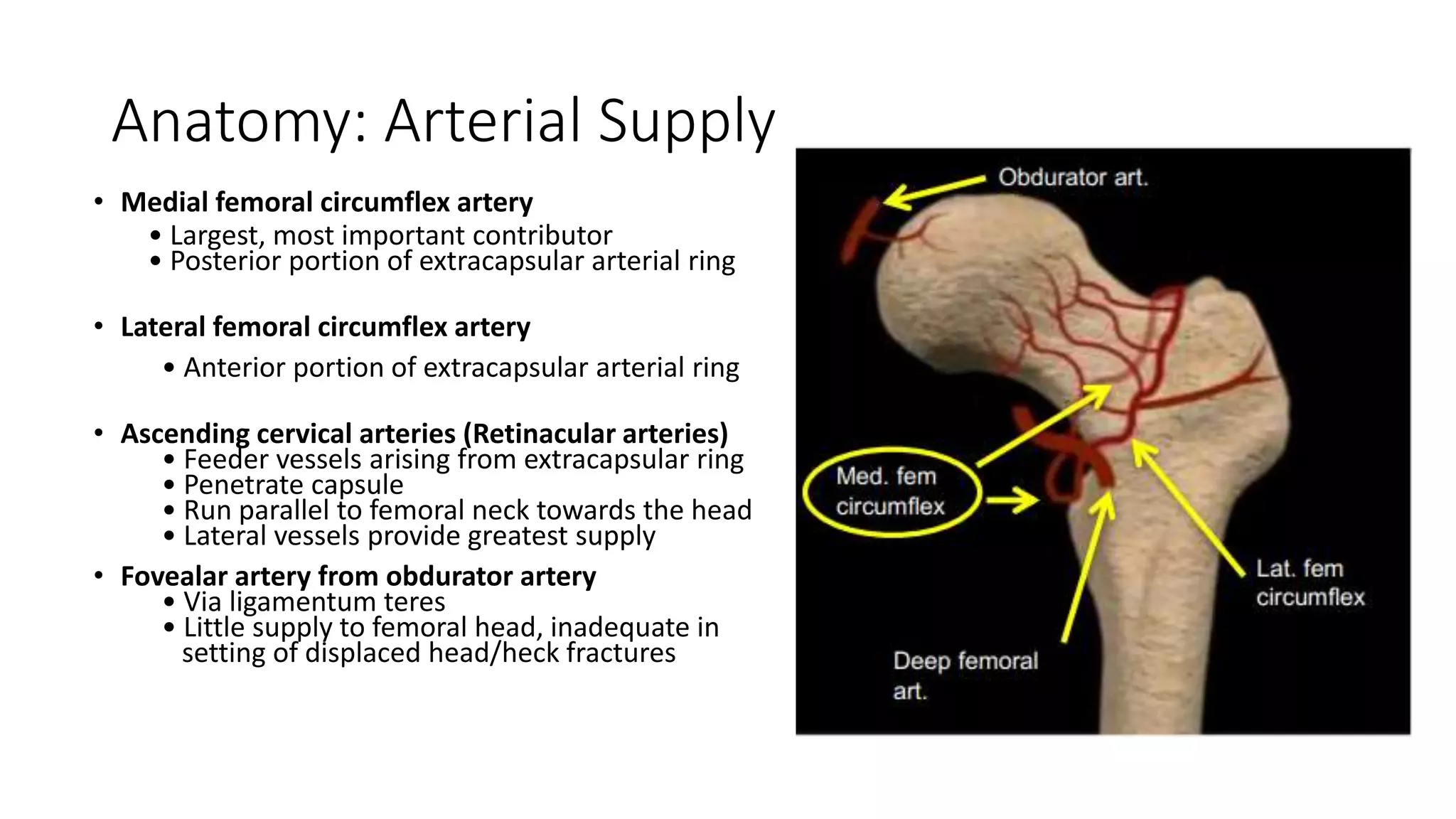
1. Proximal femur fractures are divided into femoral head, femoral neck, and extracapsular fractures based on location. Accurately classifying the fracture type guides surgical management.
2. Femoral neck fractures occur through the intra-capsular part of the femoral neck. They are classified using the Garden or Pauwel's classifications which determine stability and treatment approach.
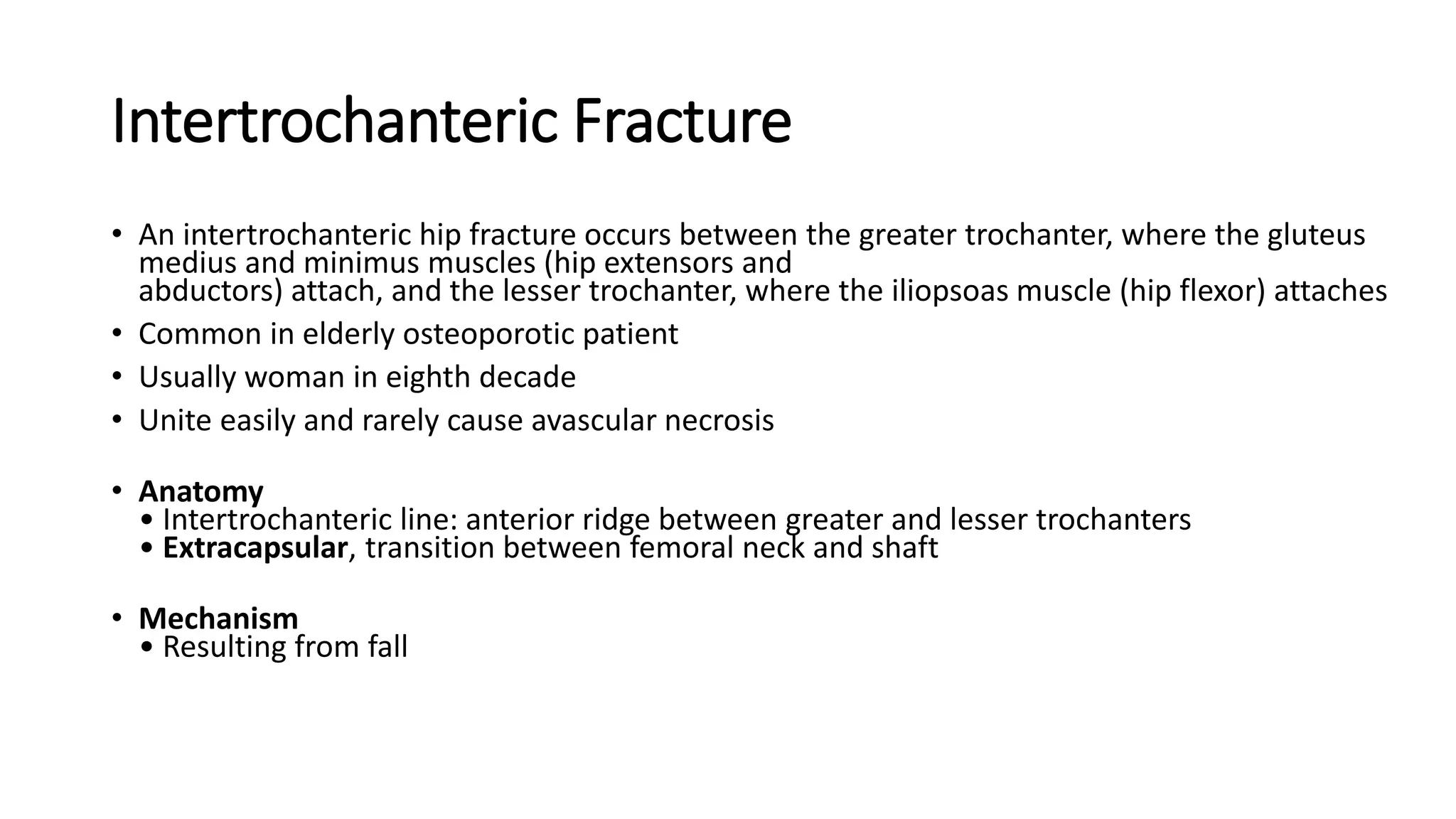
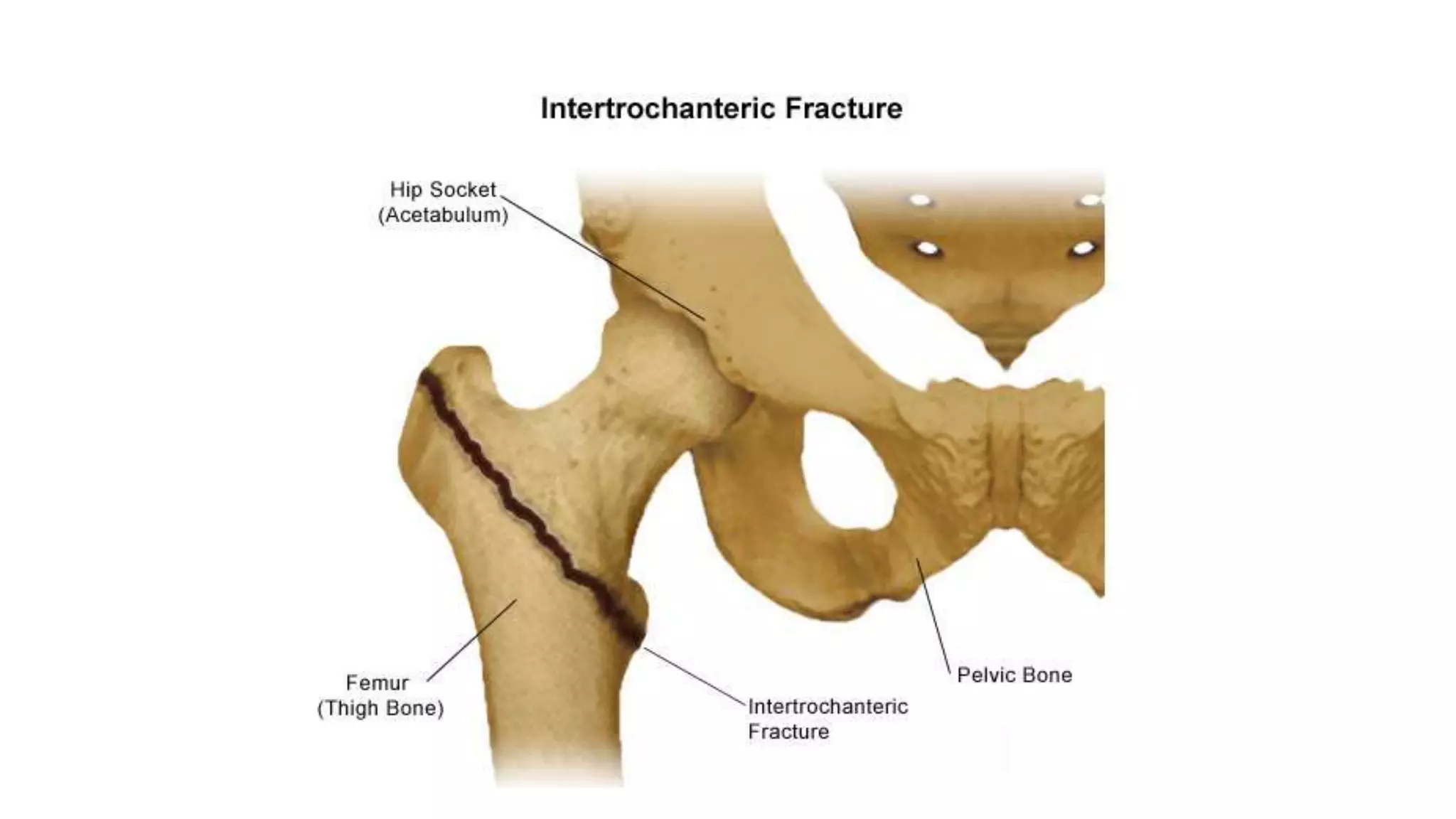
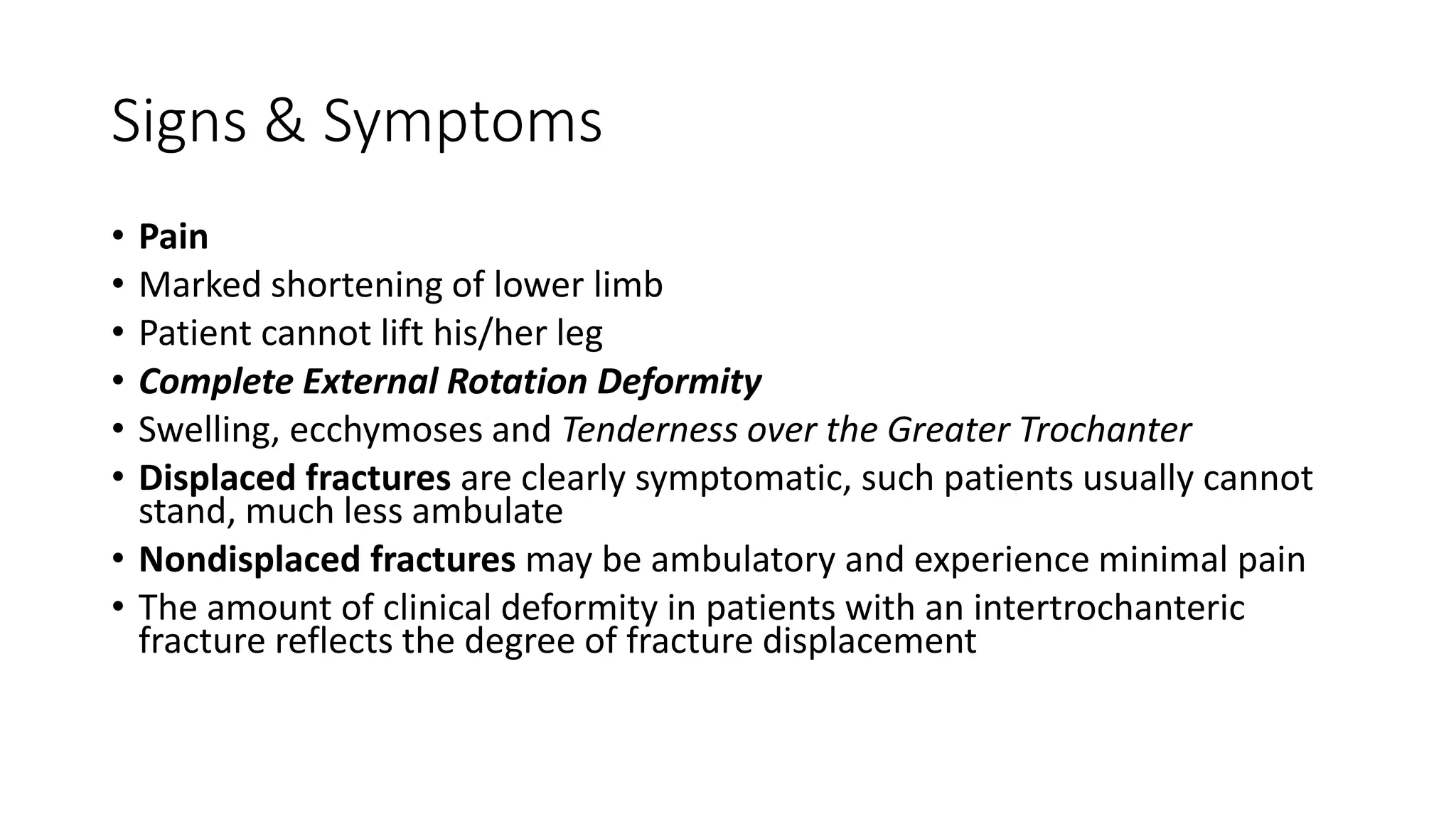
3. Intertrochanteric fractures occur between the greater and lesser trochanters. Younger patients often experience high-energy injuries while the elderly commonly sustain them from falls. Treatment depends on the Evans classification and stability.