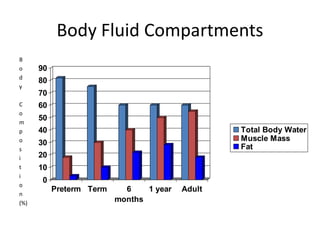
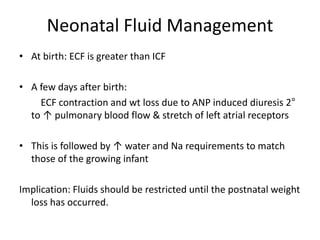
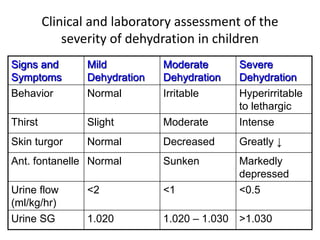
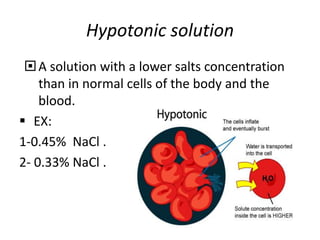
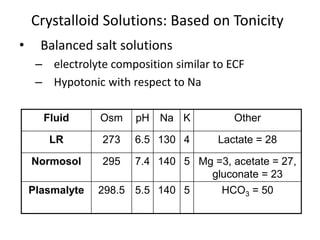
This document discusses pediatric fluid therapy and body fluid compartments. It begins by describing the different fluid compartments in the body, including total body water, extracellular fluid, and intracellular fluid. It then focuses on neonatal fluid management, noting that extracellular fluid is initially greater than intracellular fluid at birth, and describing appropriate intravenous fluid volumes for neonates. The document also discusses fluid requirements in children, evaluation of intravascular volume, choice of fluid types including crystalloids, colloids, and blood products, and provides guidelines for fluid resuscitation in dehydrated children.