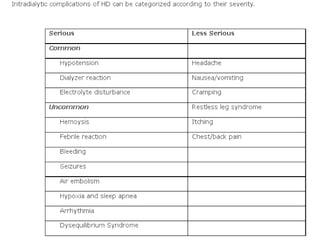
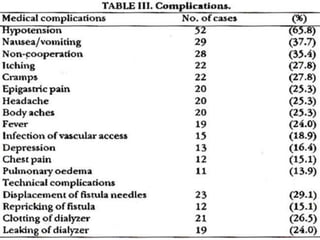
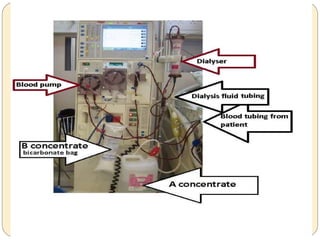
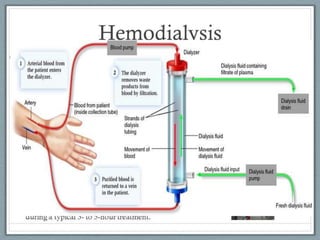
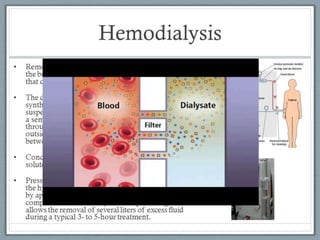
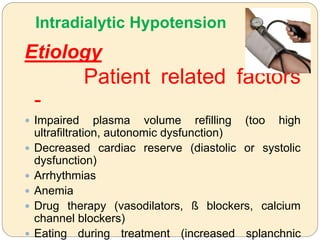
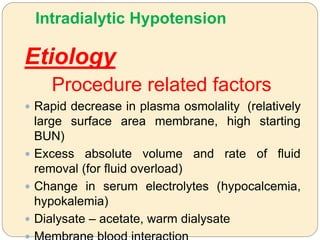
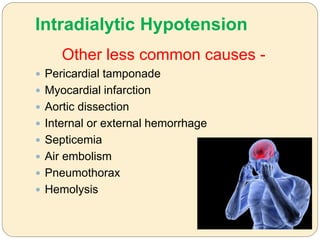
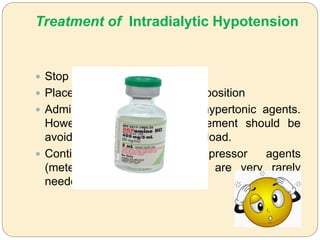
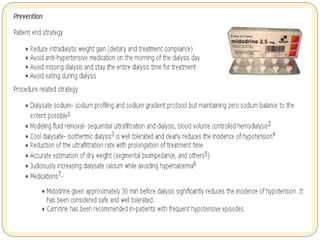
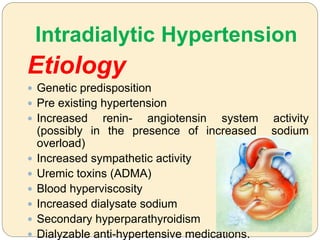
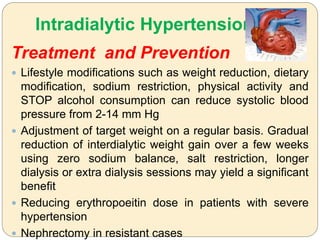
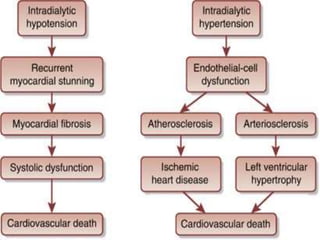
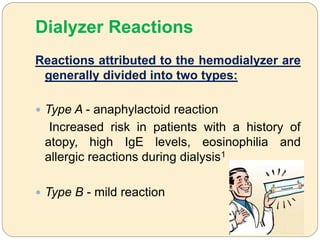
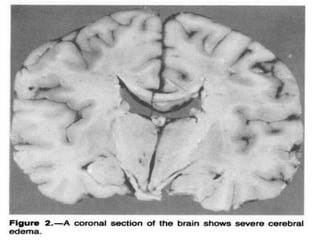
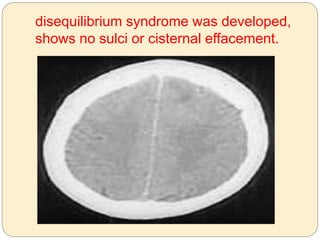
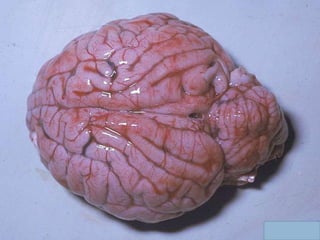
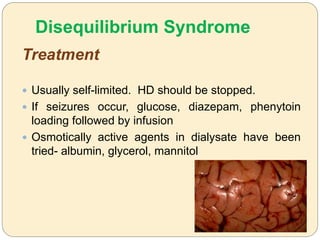
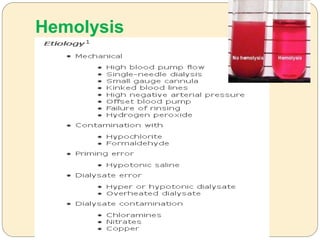
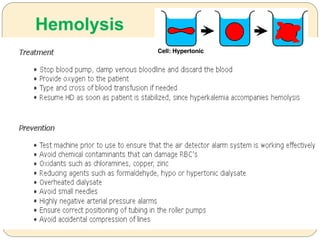
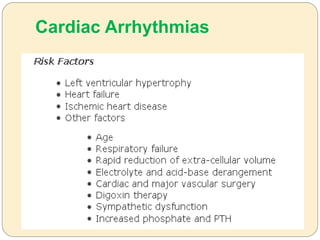
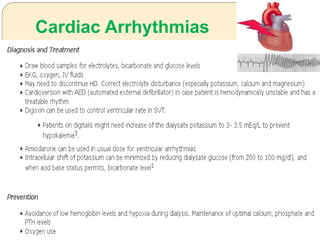
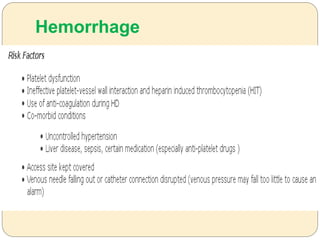
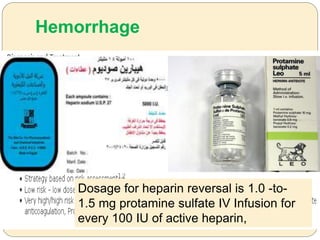
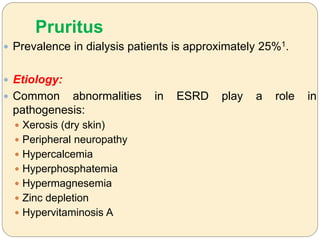
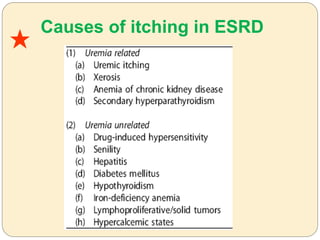
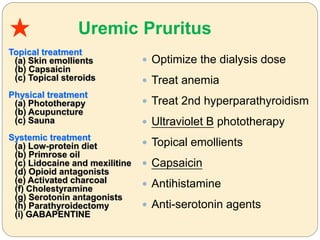
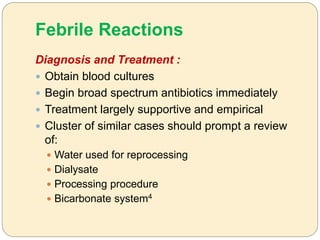
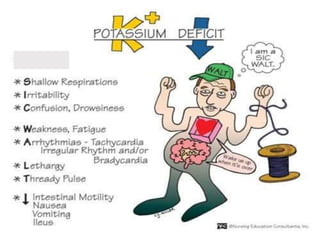
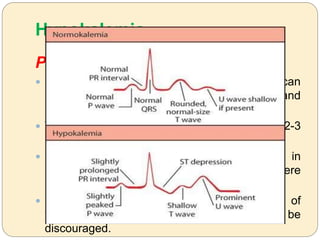
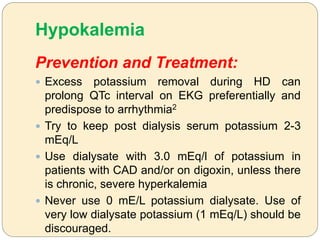
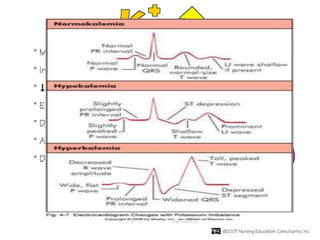
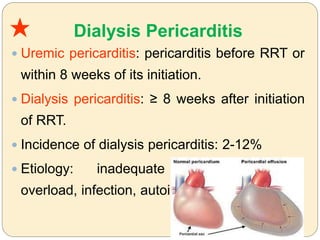
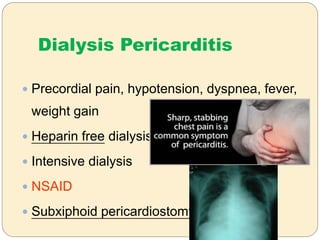
The document discusses various complications that can occur during hemodialysis treatment including intradialytic hypotension, dialyzer reactions, disequilibrium syndrome, cramping, air embolism, hemolysis, cardiac arrhythmias, hemorrhage, pruritus, febrile reactions, hypokalemia, hyperkalemia, and dialysis pericarditis. It describes the etiology, diagnosis, and treatment approaches for each complication.