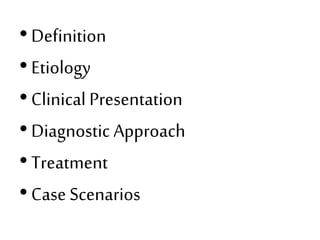
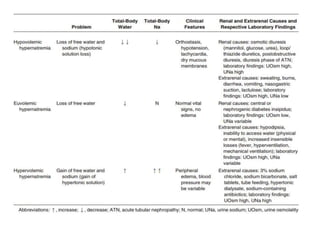
Hypernatremia is defined as a plasma sodium concentration >145 mEq/L. It is usually caused by a water deficit rather than sodium gain. Common causes include impaired thirst, diarrhea, insensible losses from fever/ventilation, and renal losses from osmotic diuresis or diabetes insipidus. Symptoms range from none in chronic cases to neurologic issues like altered mental status. Treatment involves gradually correcting the sodium level by about 10-12 mEq/L/day using oral or IV water while monitoring for complications like cerebral edema. Replacing volume deficits and identifying underlying causes are also important.
![• Hypernatremia due to water loss
The loss of water must occur in excess of
electrolyte losses in order to raise [Na].
Nonrenal water loss may be due to
evaporation from the skin and respiratory
tract (insensible losses) or loss from the GI
tract.
Diarrhea is the most common GI cause of
hypernatremia.](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-7-320.jpg)
![• Hypernatremia secondary to nonosmotic urinary
water loss is usually caused by
(a) impaired vasopressin secretion (central
diabetes insipidus [CDI]) or
(b) resistance to the actions of vasopressin
(nephrogenic diabetes insipidus [NDI]).
Partial defects occur more commonly than
complete defects in both types.
Patients with DI generally do not develop
hypernatremia if they are able to maintain fluid
intake adequate to compensate for the water
loss.](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-10-320.jpg)
![Clinical Presentation
• Hypernatremia results in contraction of brain cells as
water shifts to attenuate the rising ECF osmolality.
• Thus, the most severe symptoms of hypernatremia are
neurologic, including altered mental status, weakness,
neuromuscular irritability, focal neurologic deficits,
and, occasionally, coma or seizures. The presence of
encephalopathy is a poor prognostic sign in
hypernatremia, and carries a mortality rate as high as
50%.
• As with hyponatremia, the severity of the clinical
manifestations is related to the acuity and magnitude
of the rise in plasma [Na].](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-18-320.jpg)


![• Chronic asymptomatic hypernatremia
The risk of treatment-related complication is
increased due to the cerebral adaptation to
the chronic hyperosmolar state, and the
plasma [Na] should be lowered at a more
moderate rate (between 5 and 8 mEq/L/d).](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-39-320.jpg)
![Traditionally, correction of hypernatremia has
been accomplished by calculating free water
deficit by the equation:
Free water deficit = {([Na] - 140)/140} X (TBW)](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-41-320.jpg)
![• Alternatively,
• The change in [Na] from the administration of
1000 ml fluid can be estimated as follows:
• Because hypernatremia suggests a contraction
in water content, TBW is estimated by
multiplying lean weight (in kilograms) by 0.5 in
men (rather than 0.6) and 0.4 in women.](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-42-320.jpg)
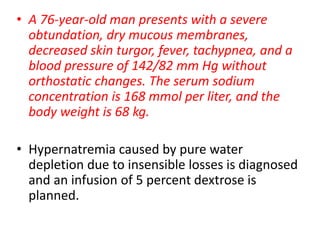
![• The estimated volume of total body water is 34 liters
(0.5X68). According to formula, the retention of 1 liter
of 5 percent dextrose will reduce the serum sodium
concentration by 4.8 mmol per liter ([0-168]÷[34+1]=-
4.8).
• The goal of treatment is to reduce the serum sodium
concentration by approximately 10 mmol per liter over
a period of 24 hours. Therefore, 2.1 liters of the
solution (10÷4.8) is required. With 1.5 liters added to
compensate for average obligatory water losses over
the 24-hour period, a total of 3.6 liters will be
administered for the next 24 hours, or 150 ml per hour.
• The serum glucose concentration will be monitored,
with insulin therapy started at the first indication of
hyperglycemia, a complication that would aggravate
the hypertonicity.](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-53-320.jpg)
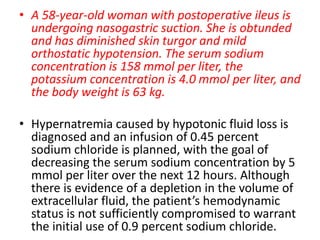
![• The estimated volume of total body water is 31.5
liters (0.5X63). It is estimated that the retention
of 1 liter of 0.45 percent sodium chloride will
reduce the serum sodium concentration by 2.5
mmol per liter ([77-158]÷[31.5+1]=-2.5). Since
the goal is to reduce the serum sodium
concentration by 5 mmol per liter over the next
12 hours, 2 liters of the solution is required
(5÷2.5).
• With 1 liter added to compensate for ongoing
losses of gastric and other fluids, a total of 3 liters
will be administered for the next 12 hours, or 250
ml per hour.](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-55-320.jpg)
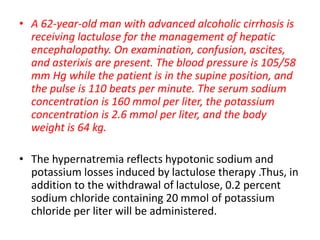
![• With the presence of ascites, the estimated
volume of total body water is about 38 liters
(0.6 X 64).
• According to the formula, the retention of 1 liter
of 0.2 percent sodium chloride containing 20
mmol of potassium chloride will reduce the
serum sodium concentration by 2.7 mmol per
liter ([(34+20)-160]÷[38+1]=-2.7). To reduce the
serum sodium concentration by 10 mmol per liter
over the next 24 hours, 3.7 liters of solution
(10÷2.7) is required.
• With 1.5 liters added to compensate for ongoing
obligatory fluid and electrolyte losses, a total of
5.2 liters will be administered](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-57-320.jpg)
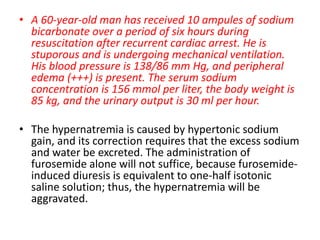
![• The administration of both furosemide and
electrolyte-free water will meet the
therapeutic goal. The estimated volume of
total body water is 51 liters (0.6X85).
• The retention of 1 liter of 5 percent dextrose is
estimated to decrease the serum sodium
concentration by 3.0 mmol per liter ([0-156]÷
[51+1]=-3.0). To reduce the serum sodium
concentration by 6.0 mmol per liter over a
period of eight hours, 2.0 liters of 5 percent
dextrose will be infused at a rate of 250 ml per
hour.](https://image.slidesharecdn.com/sem4hypernatremia-160623180333/85/hypernatremia-59-320.jpg)