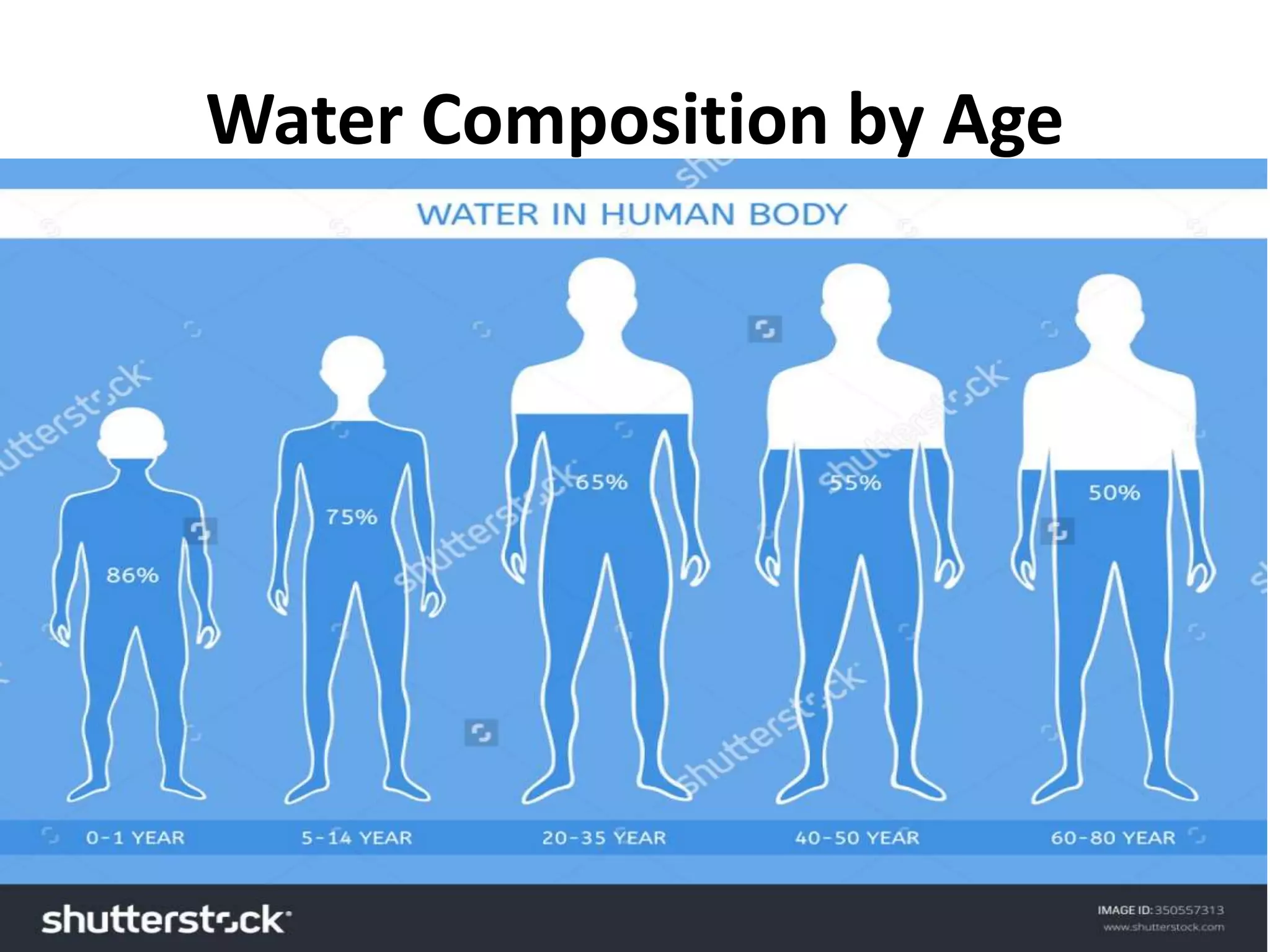
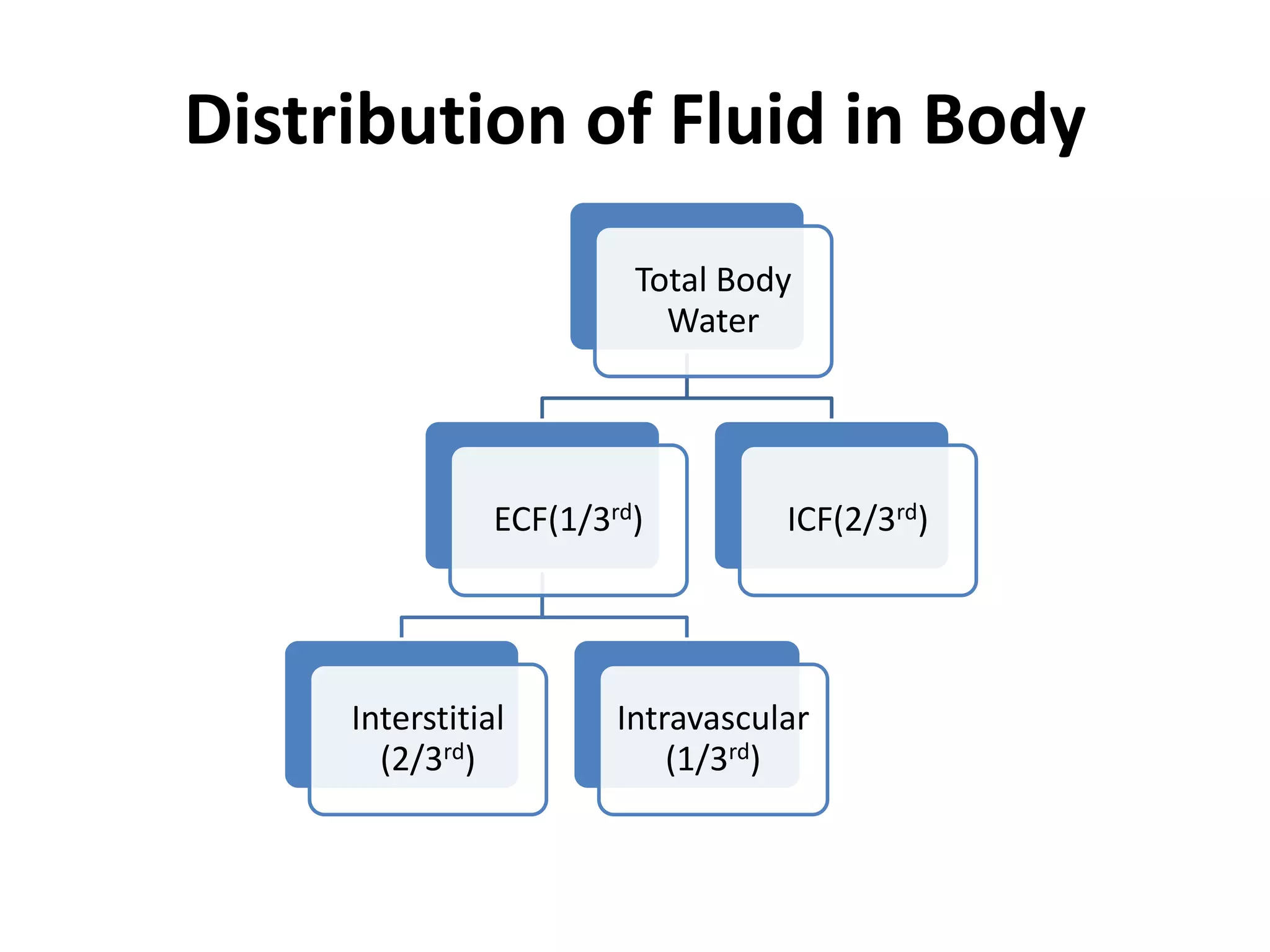
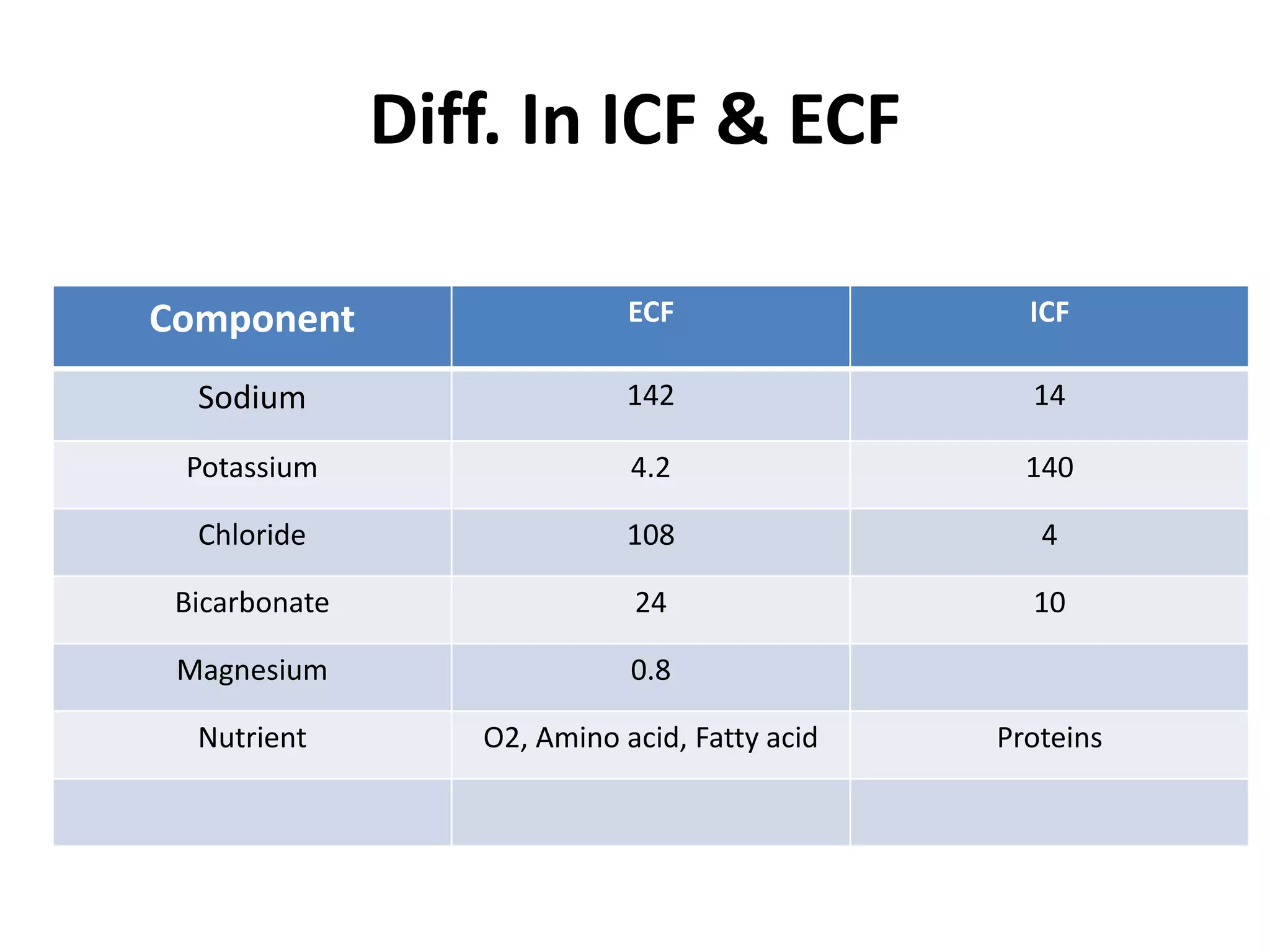
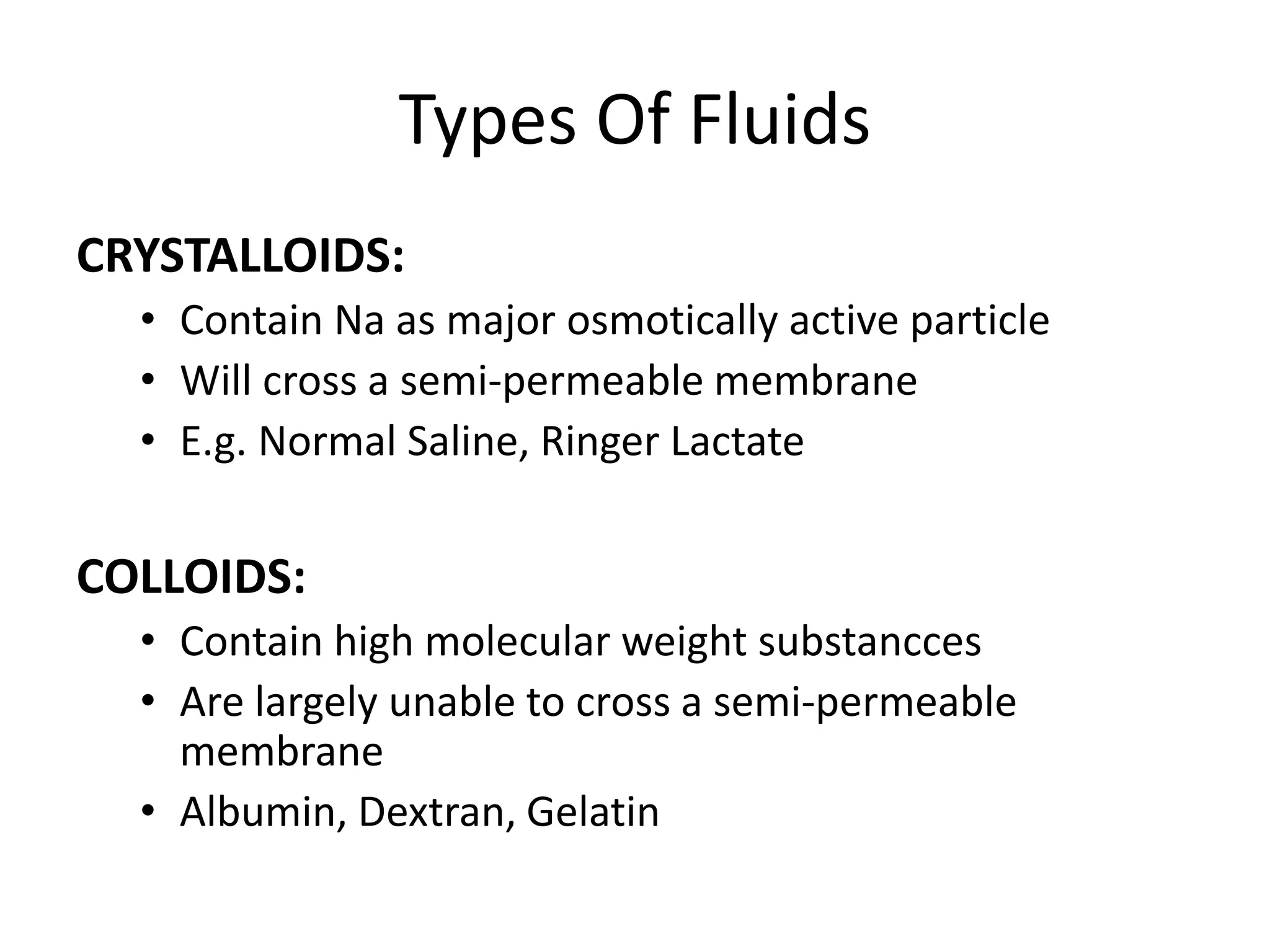
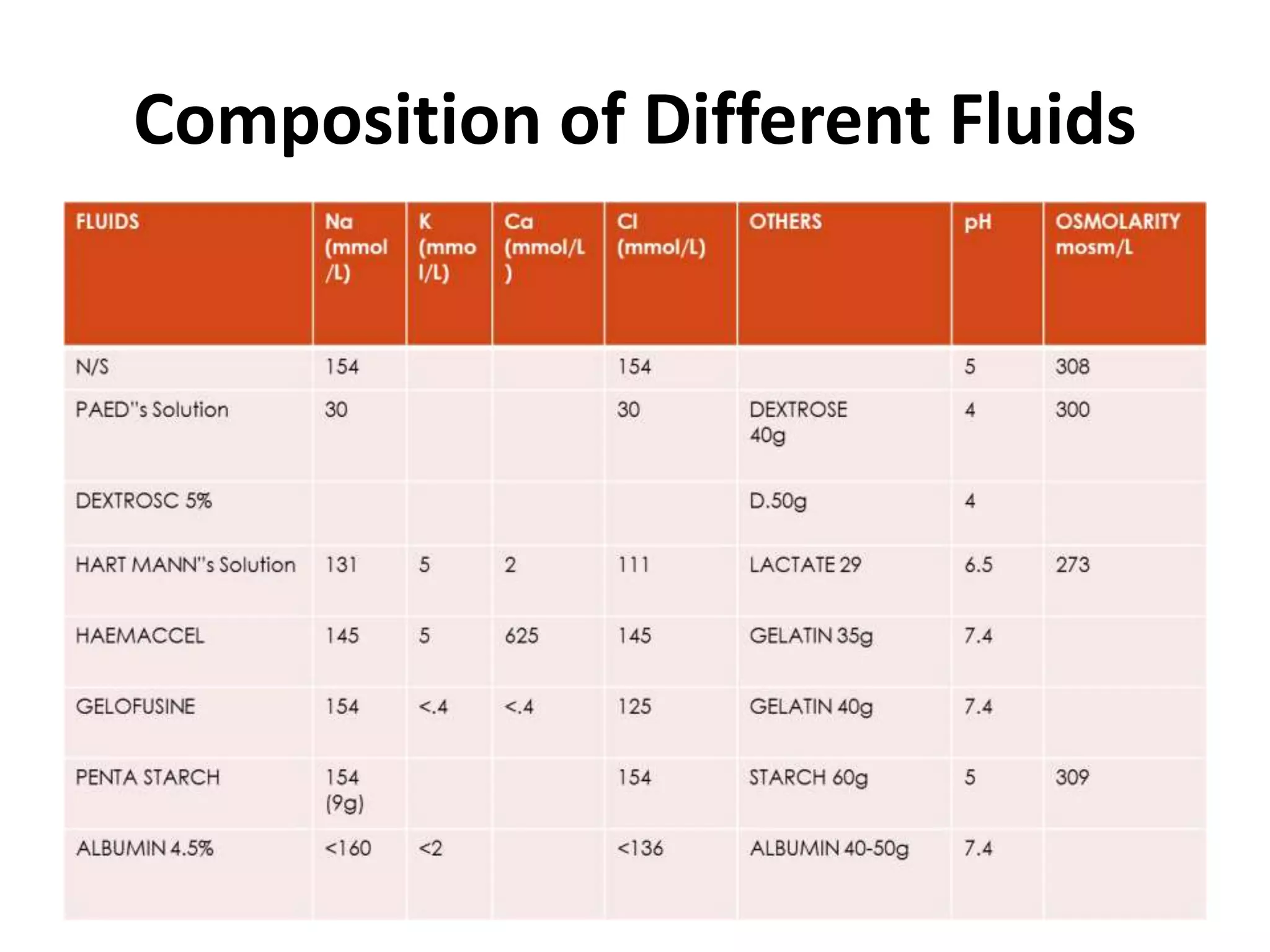
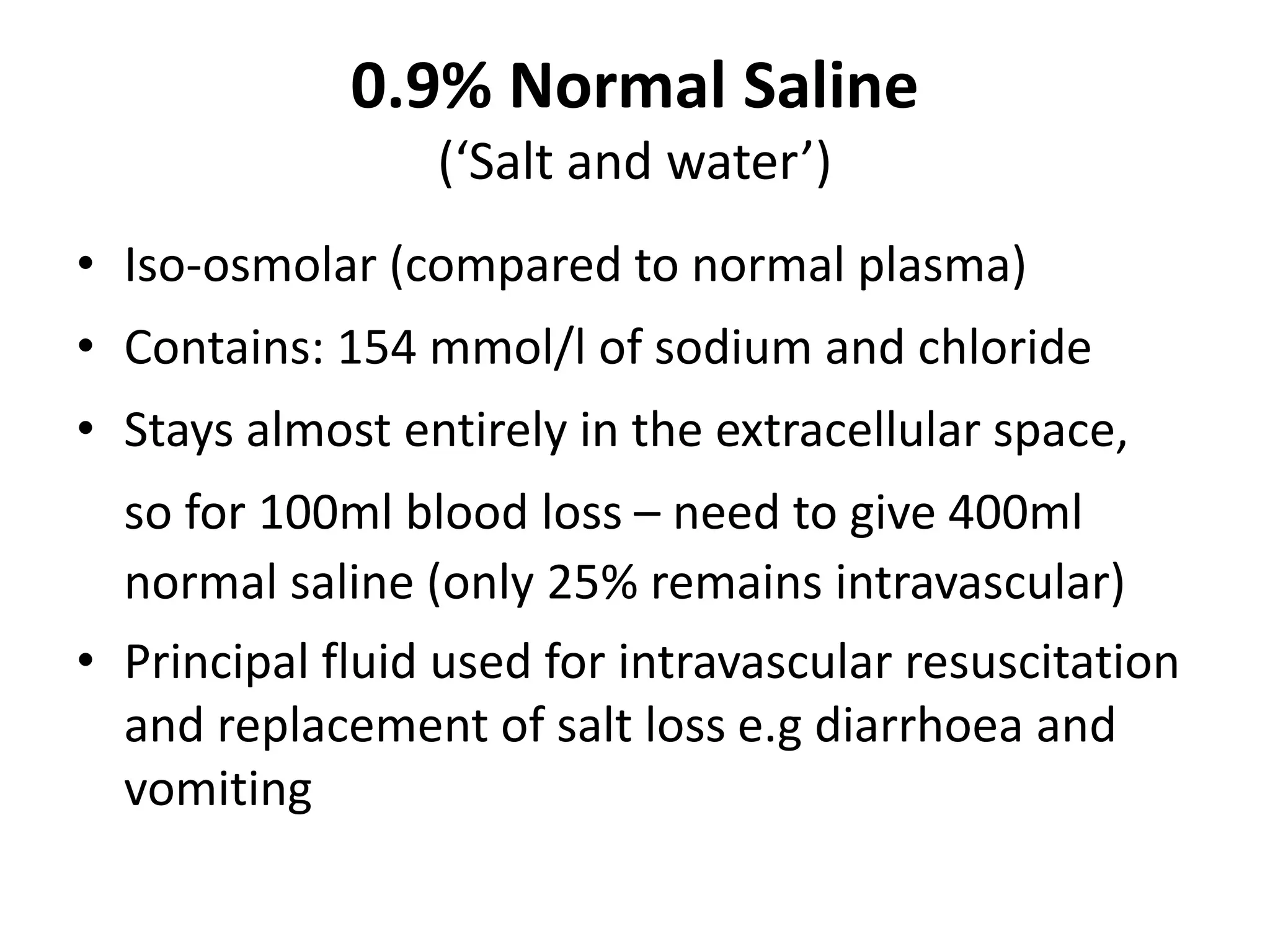
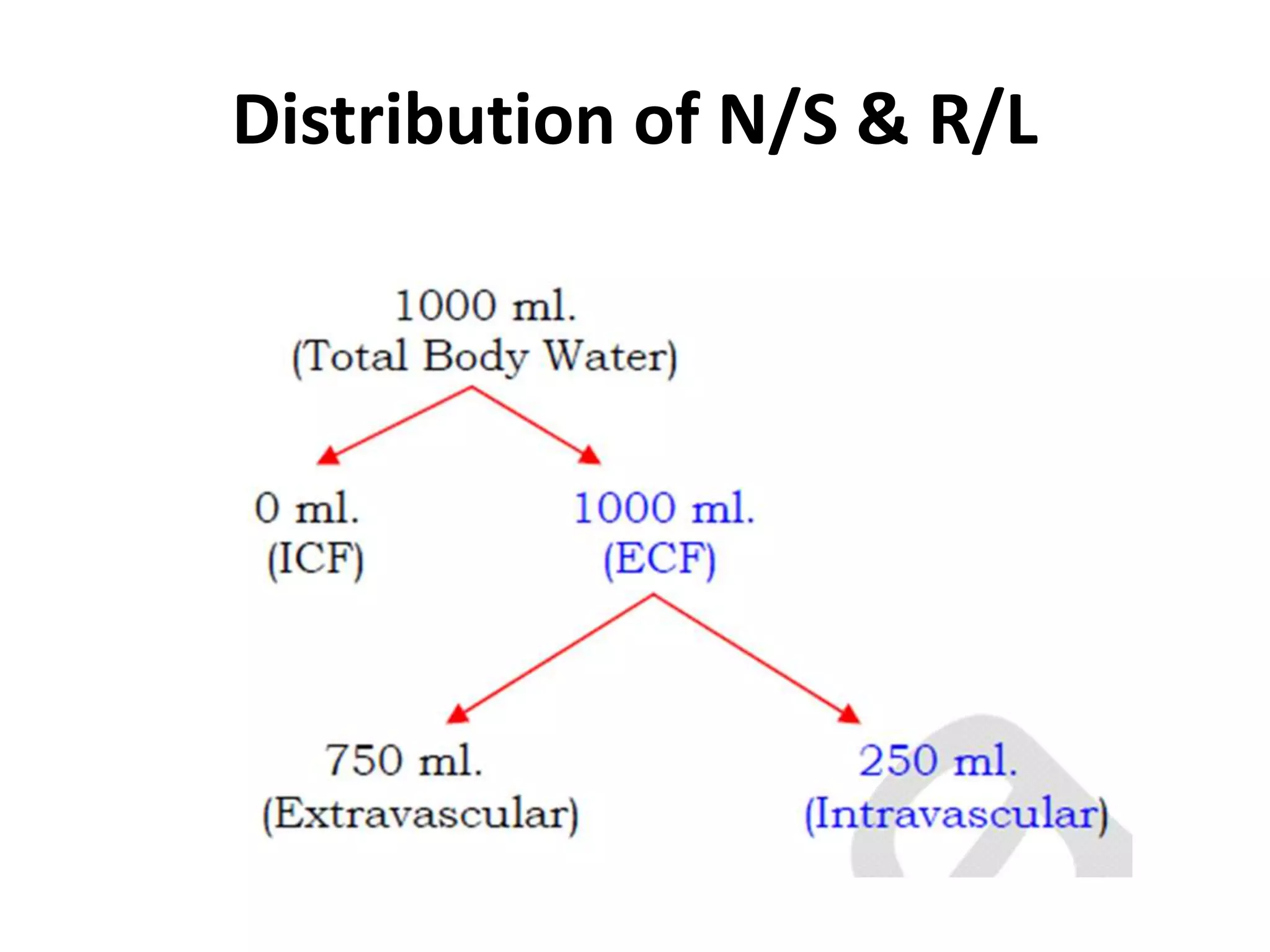
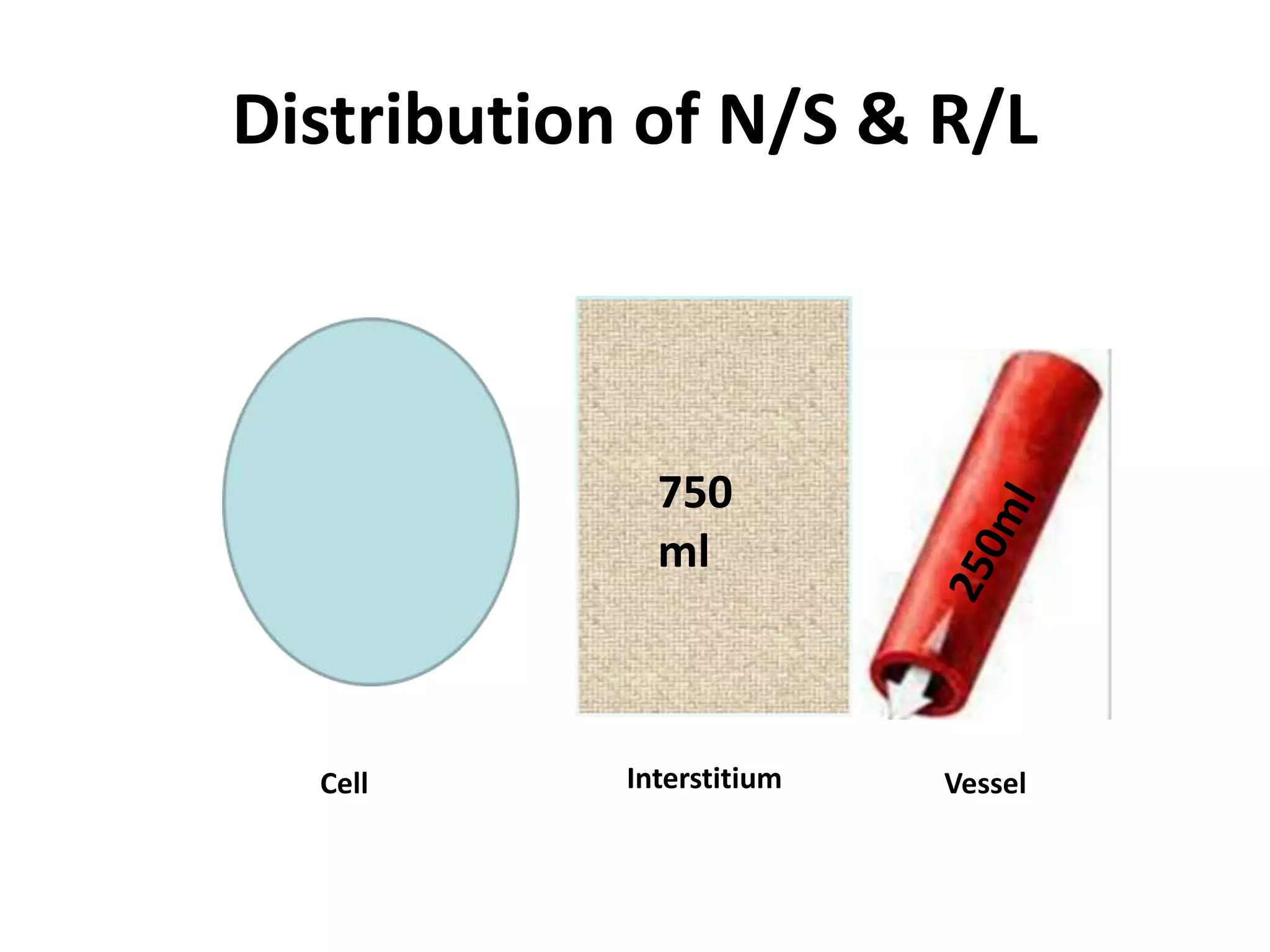
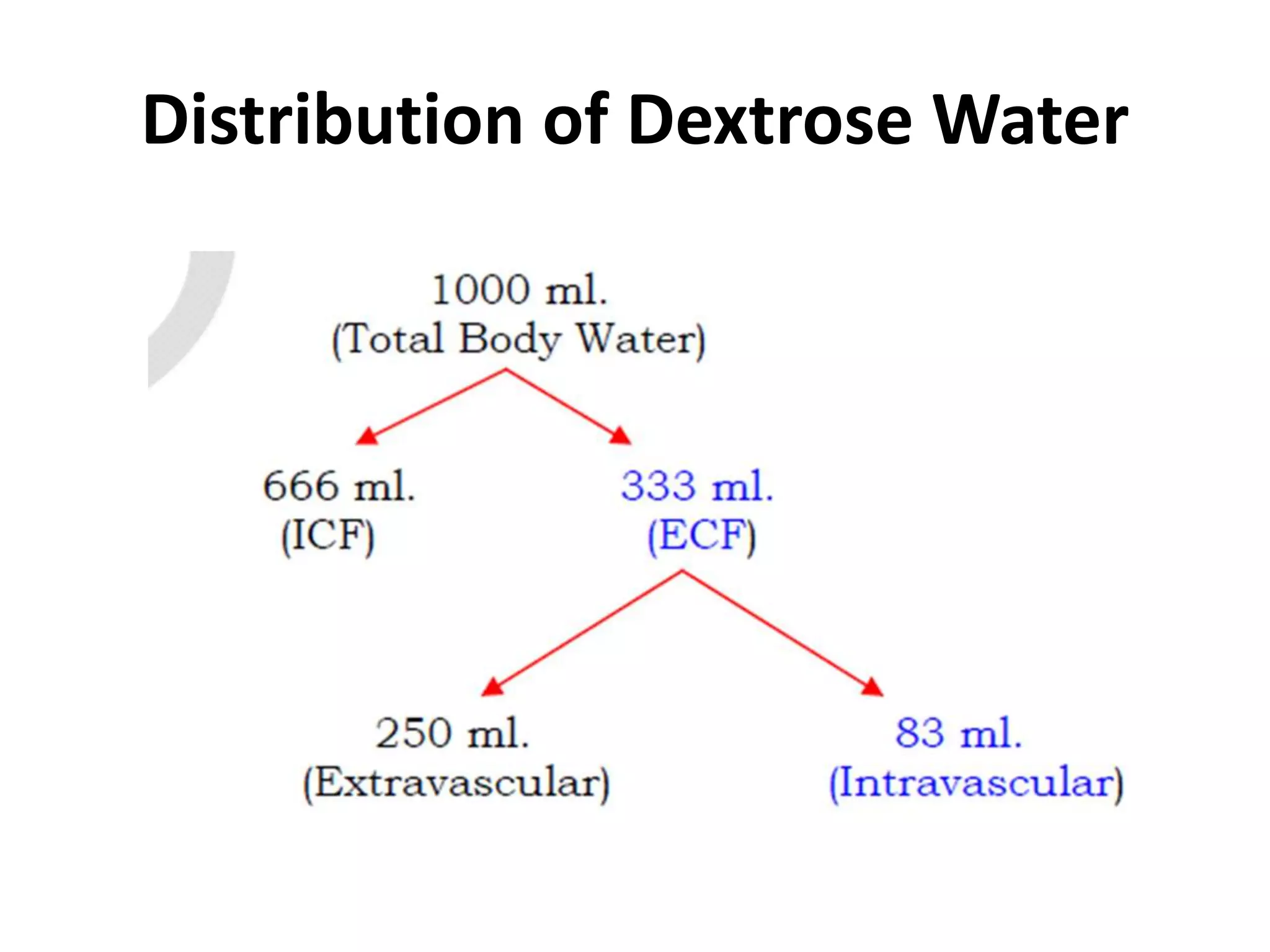
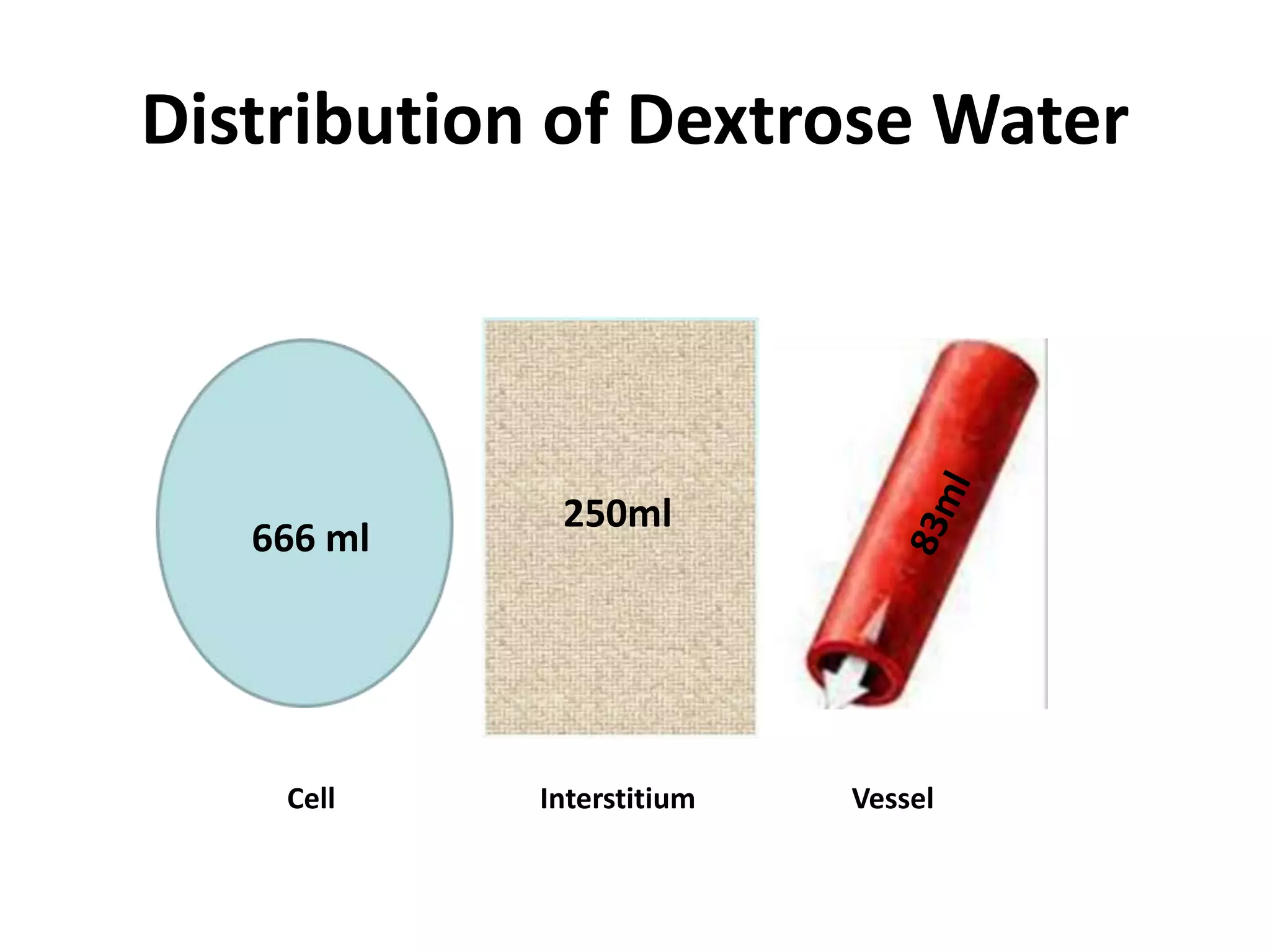
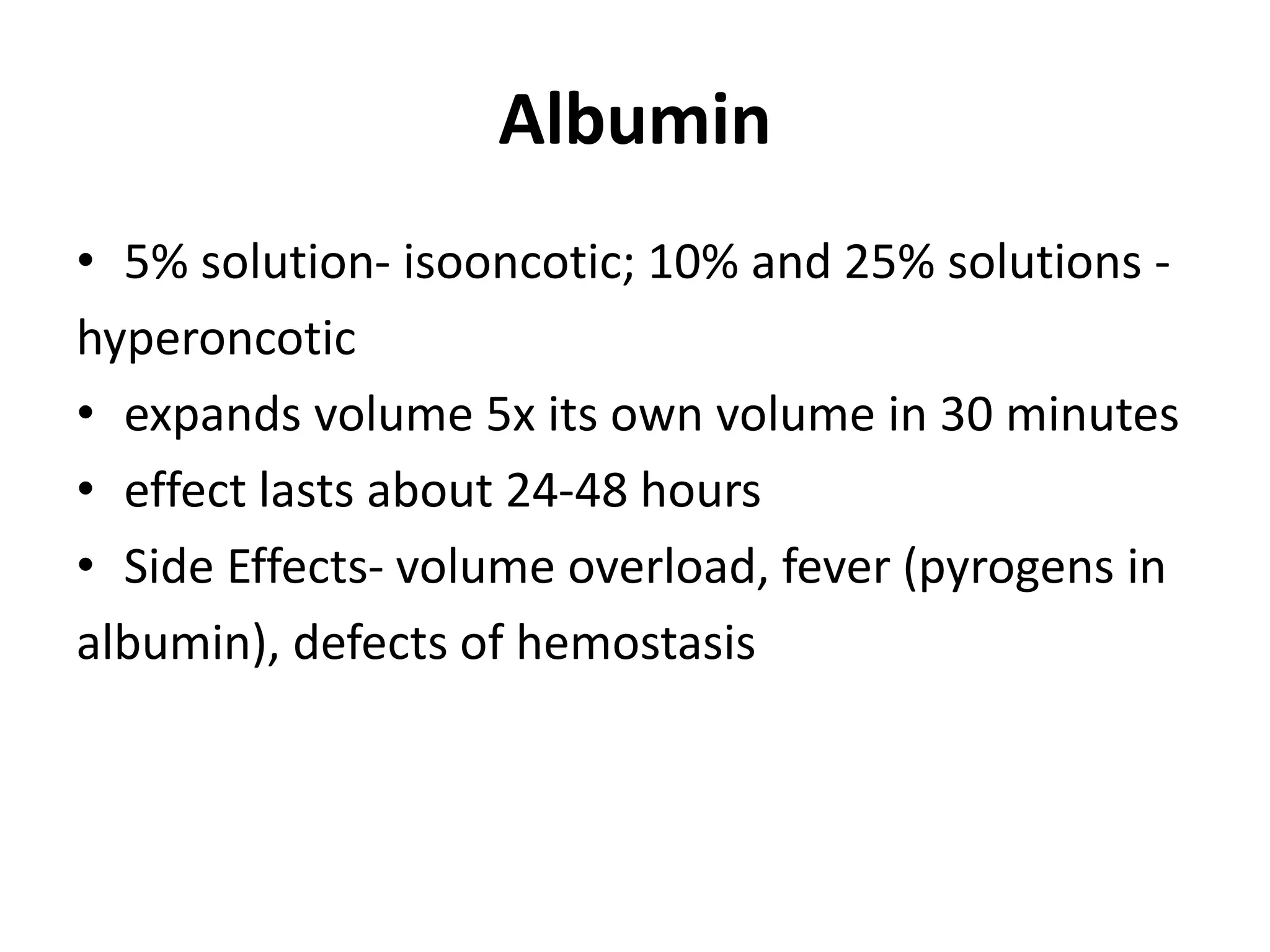
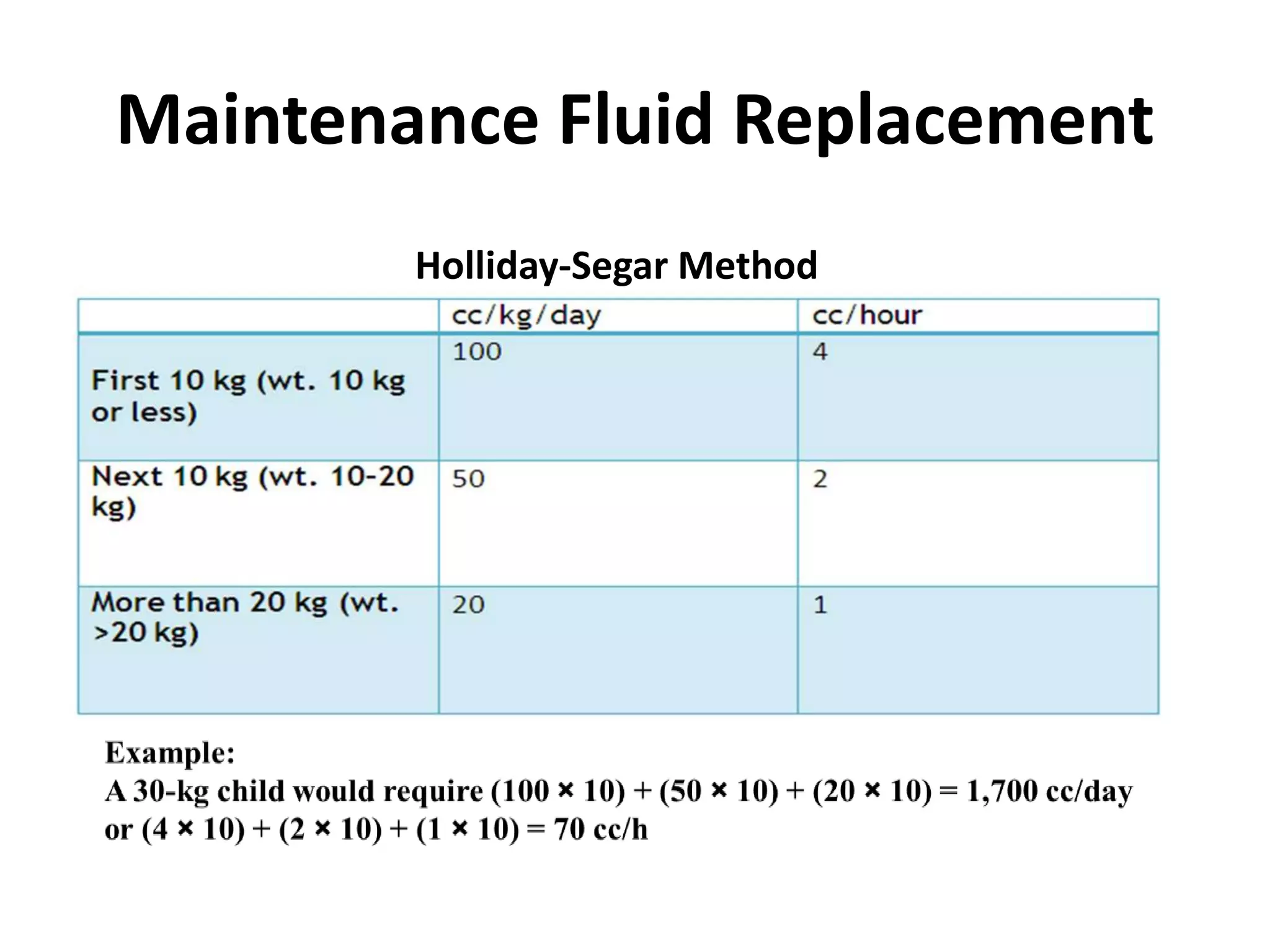
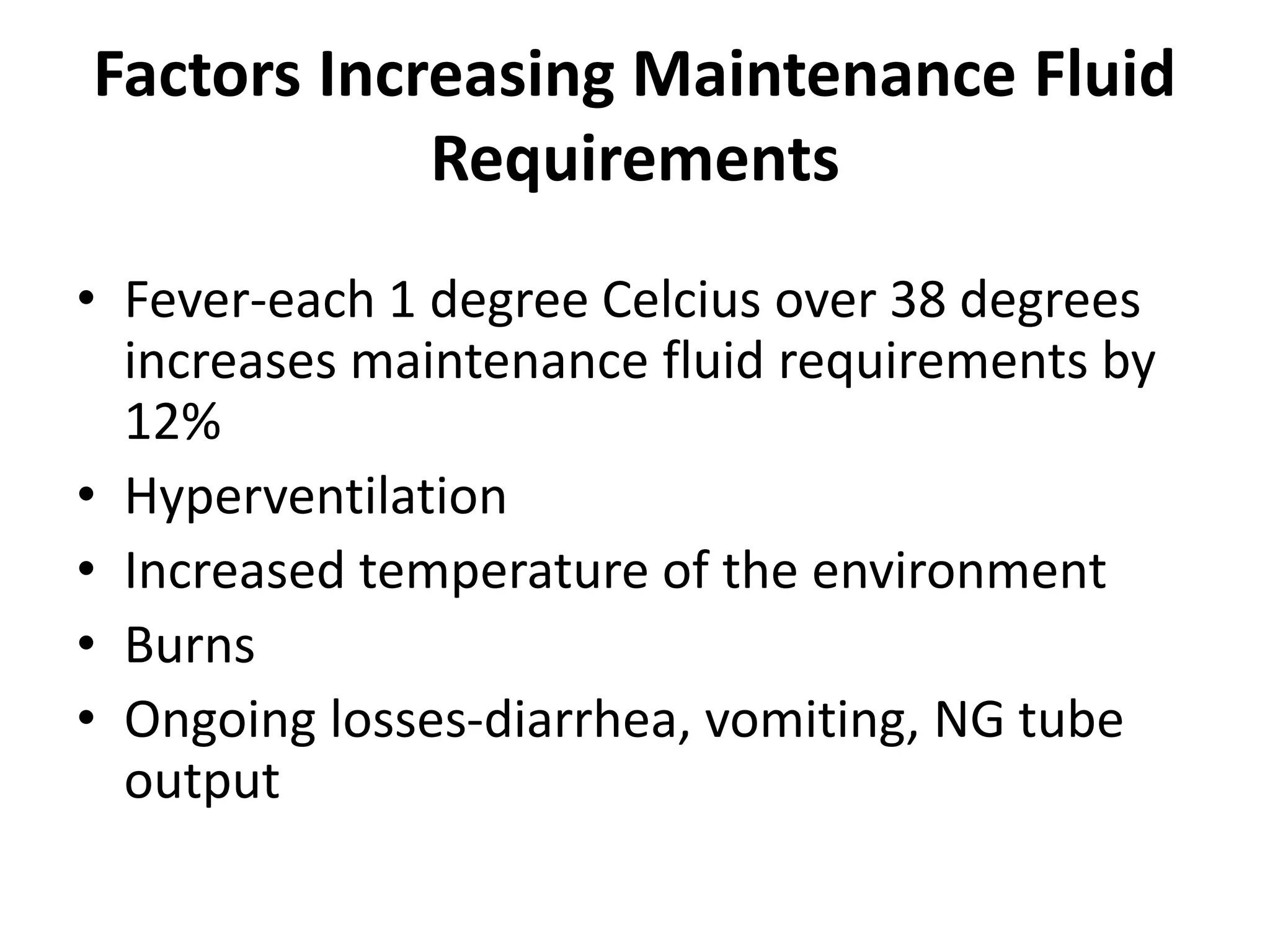
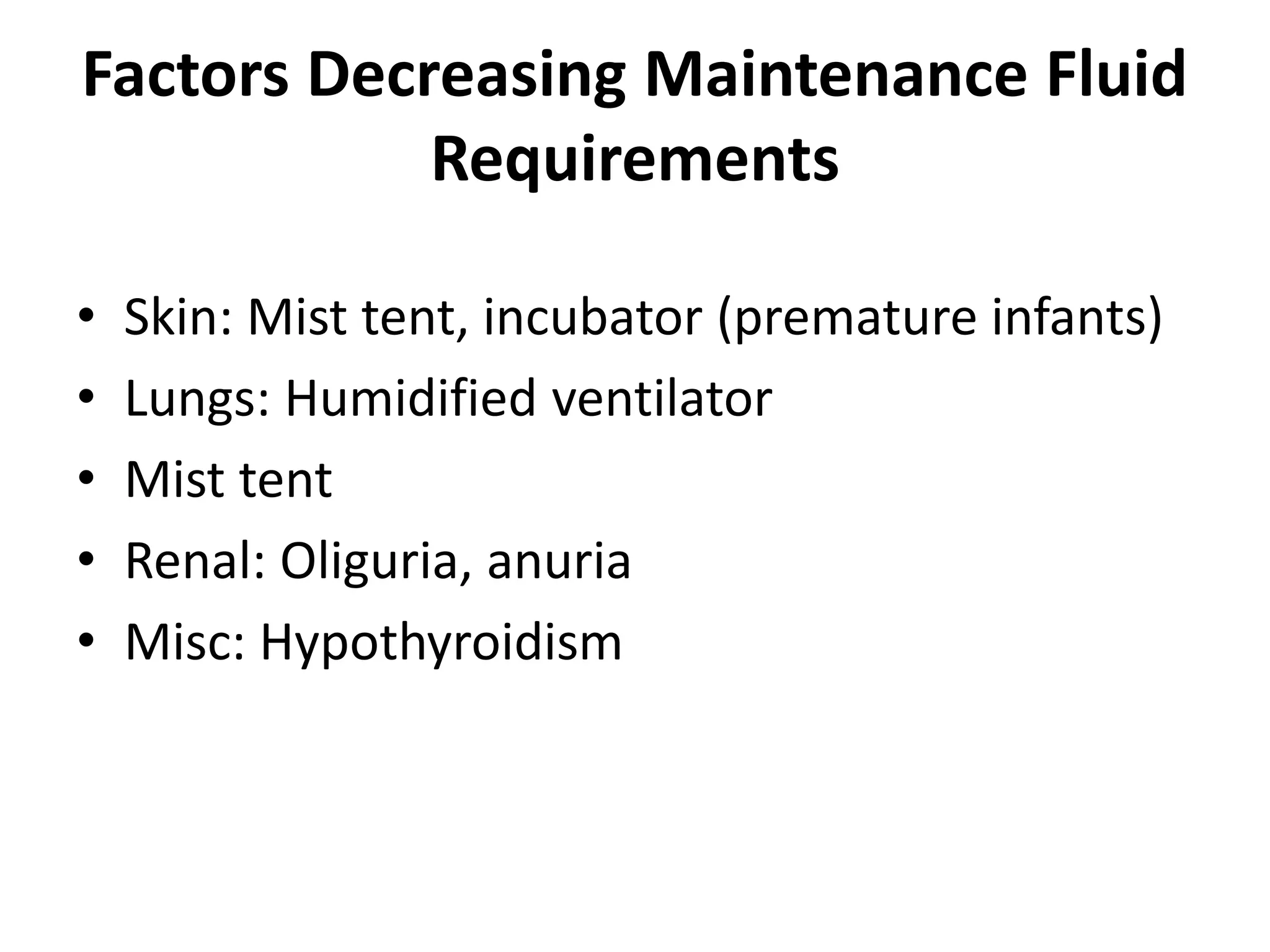
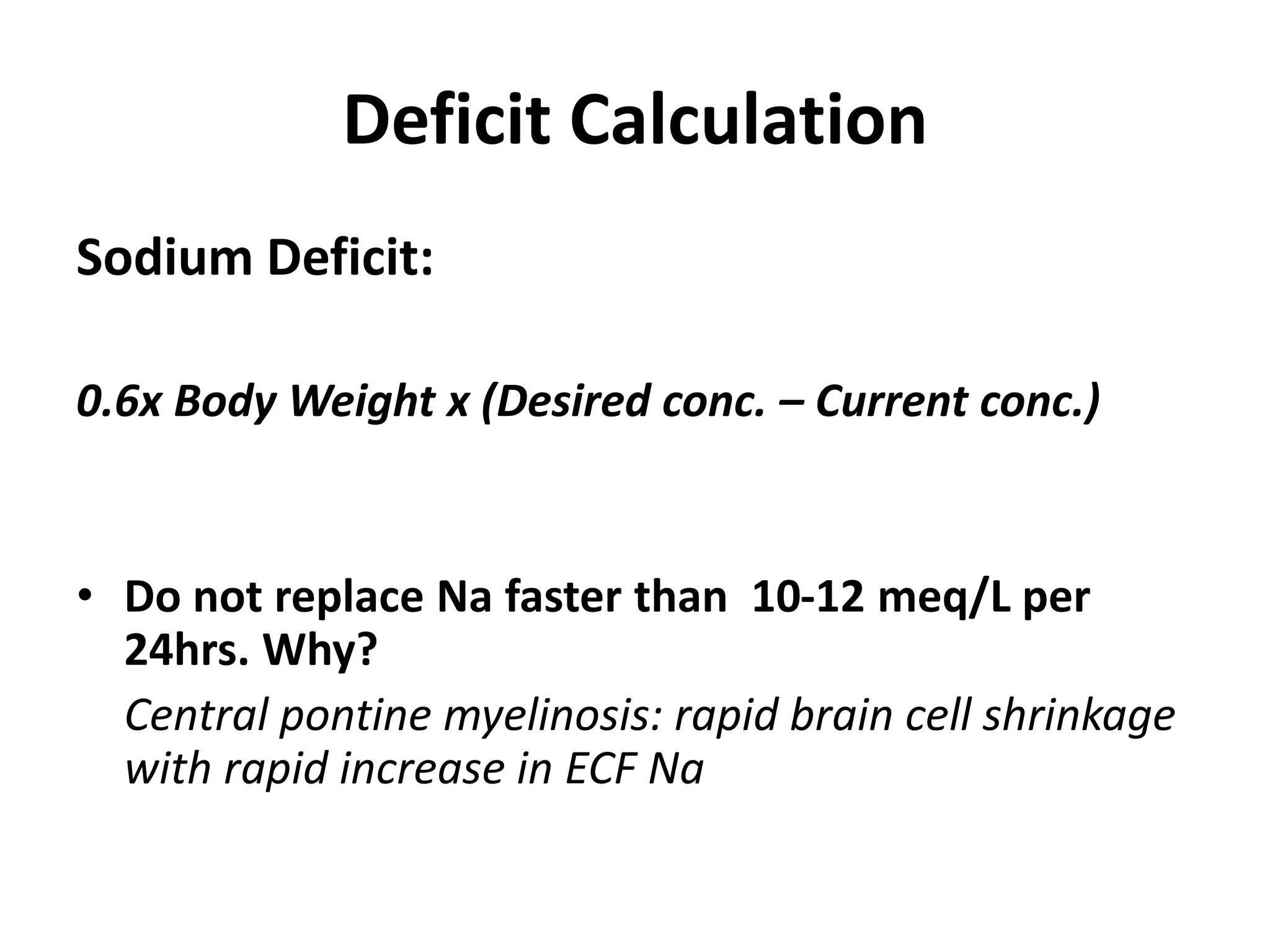
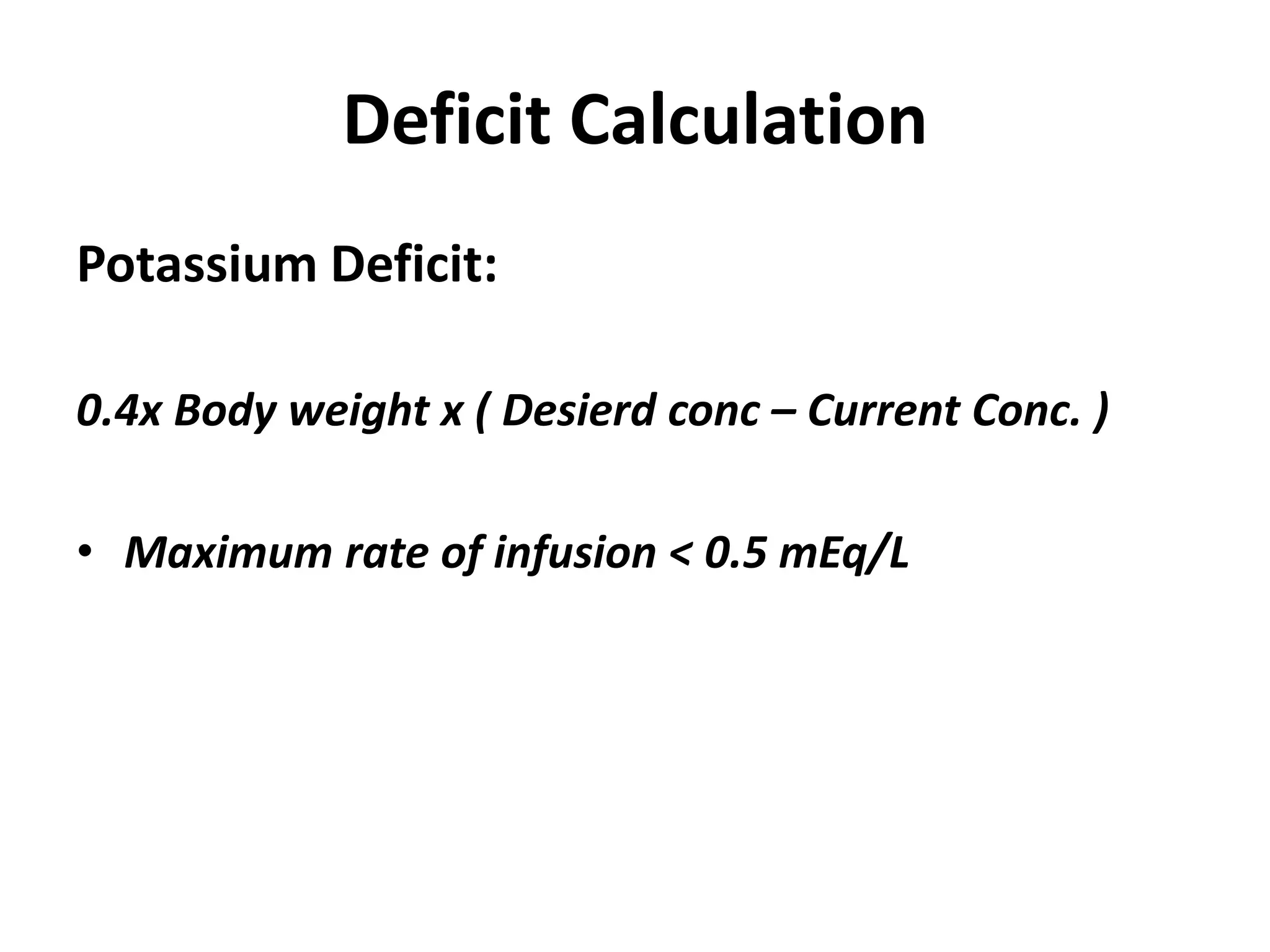
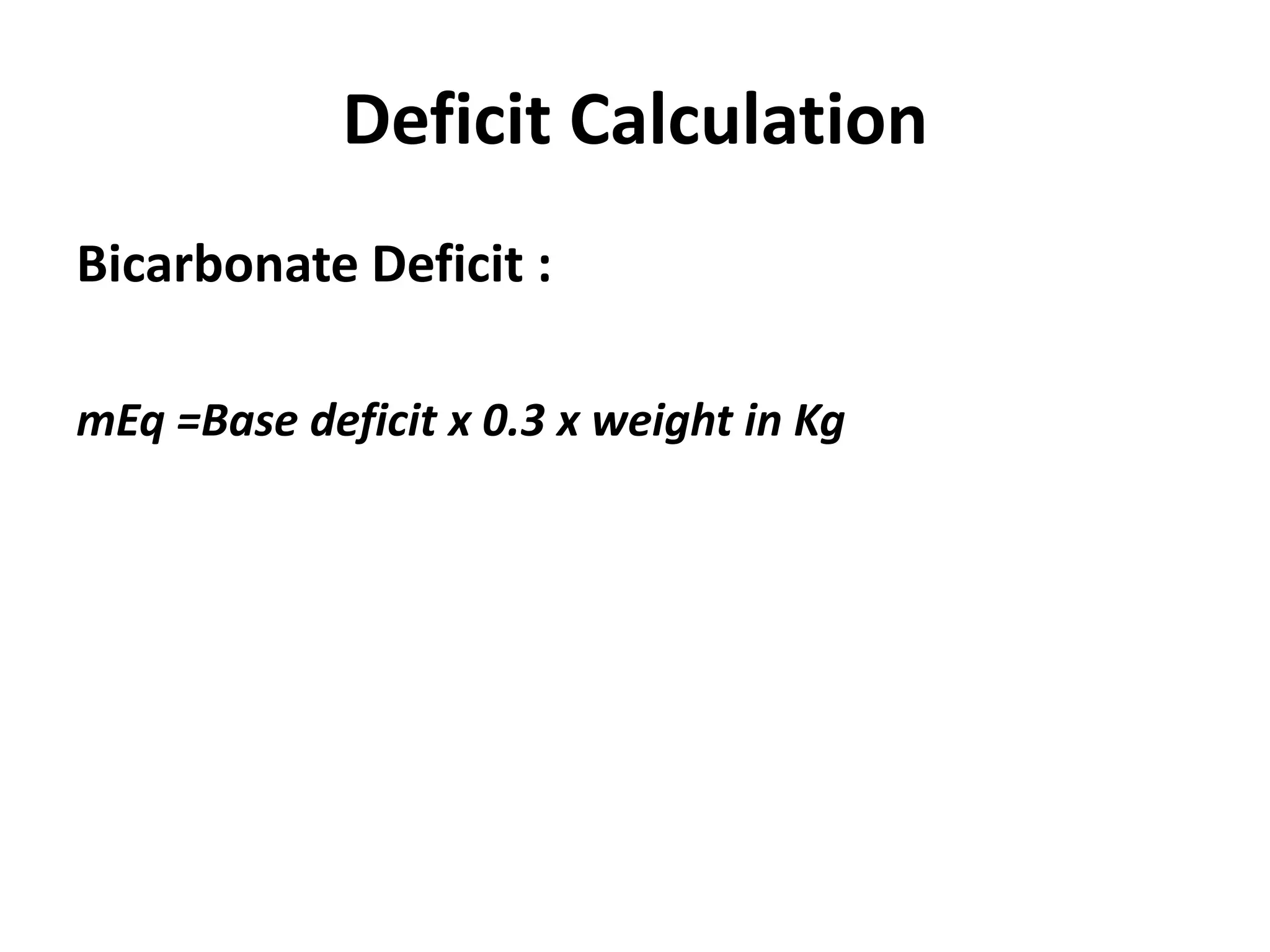
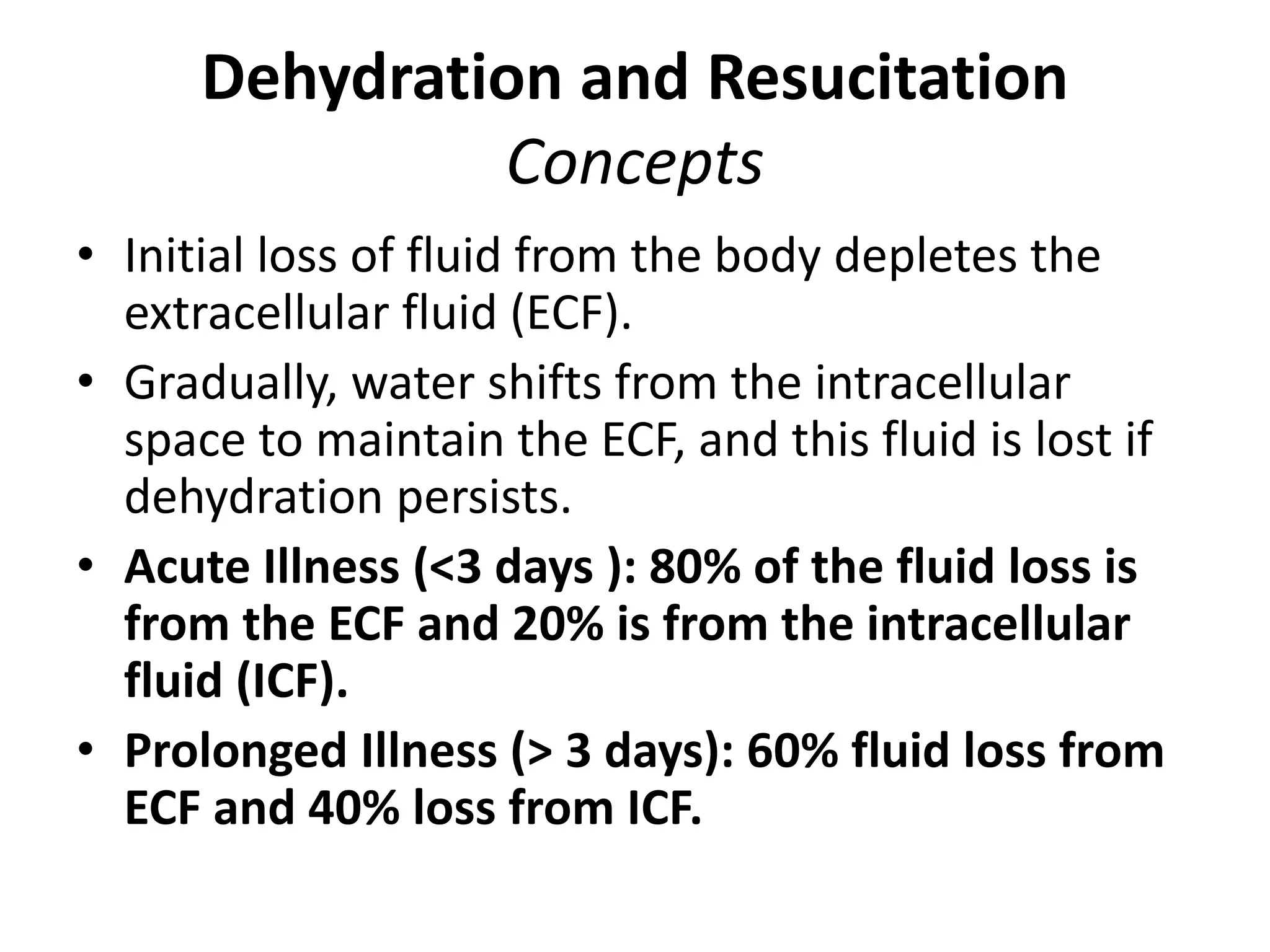
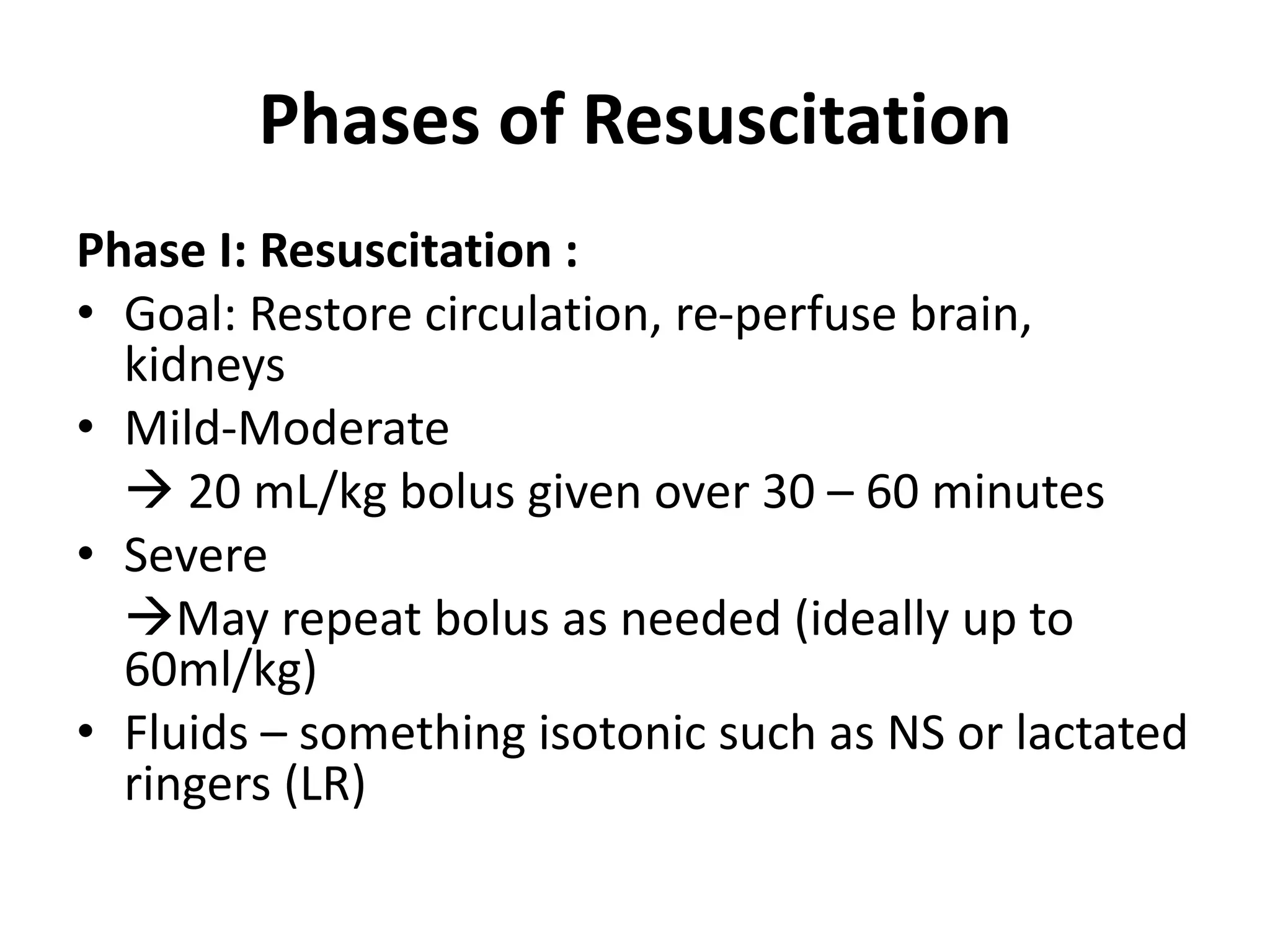
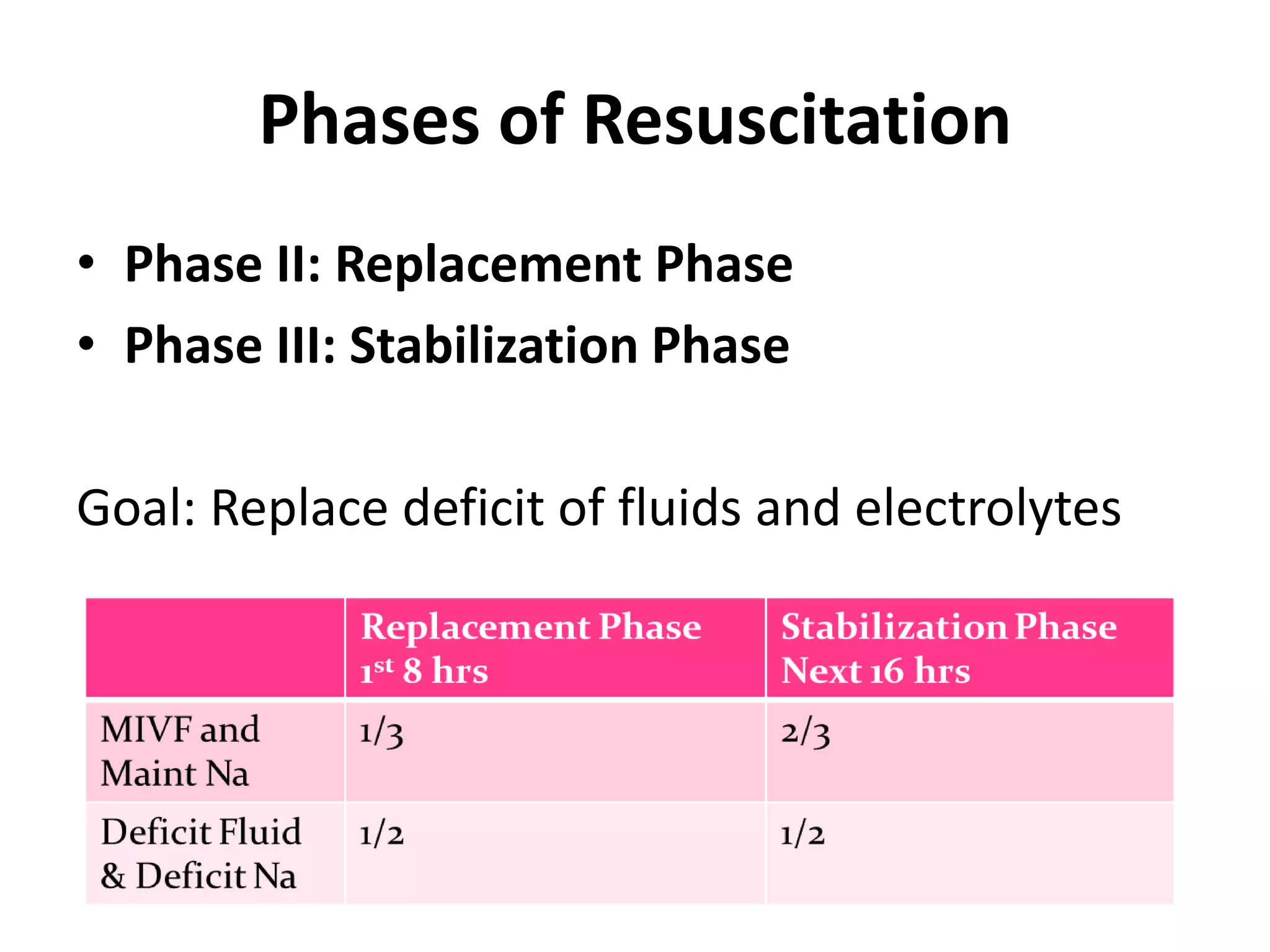
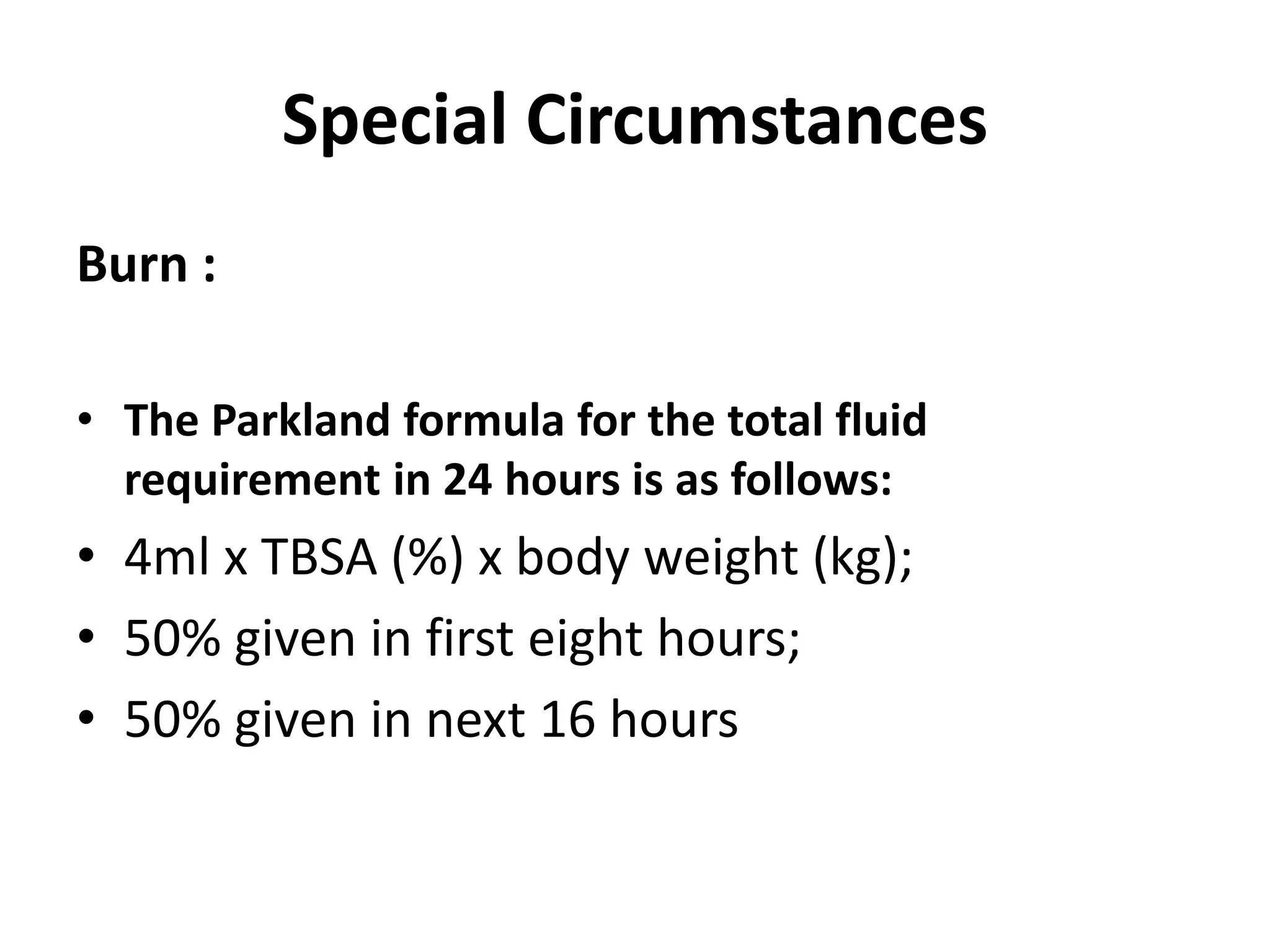
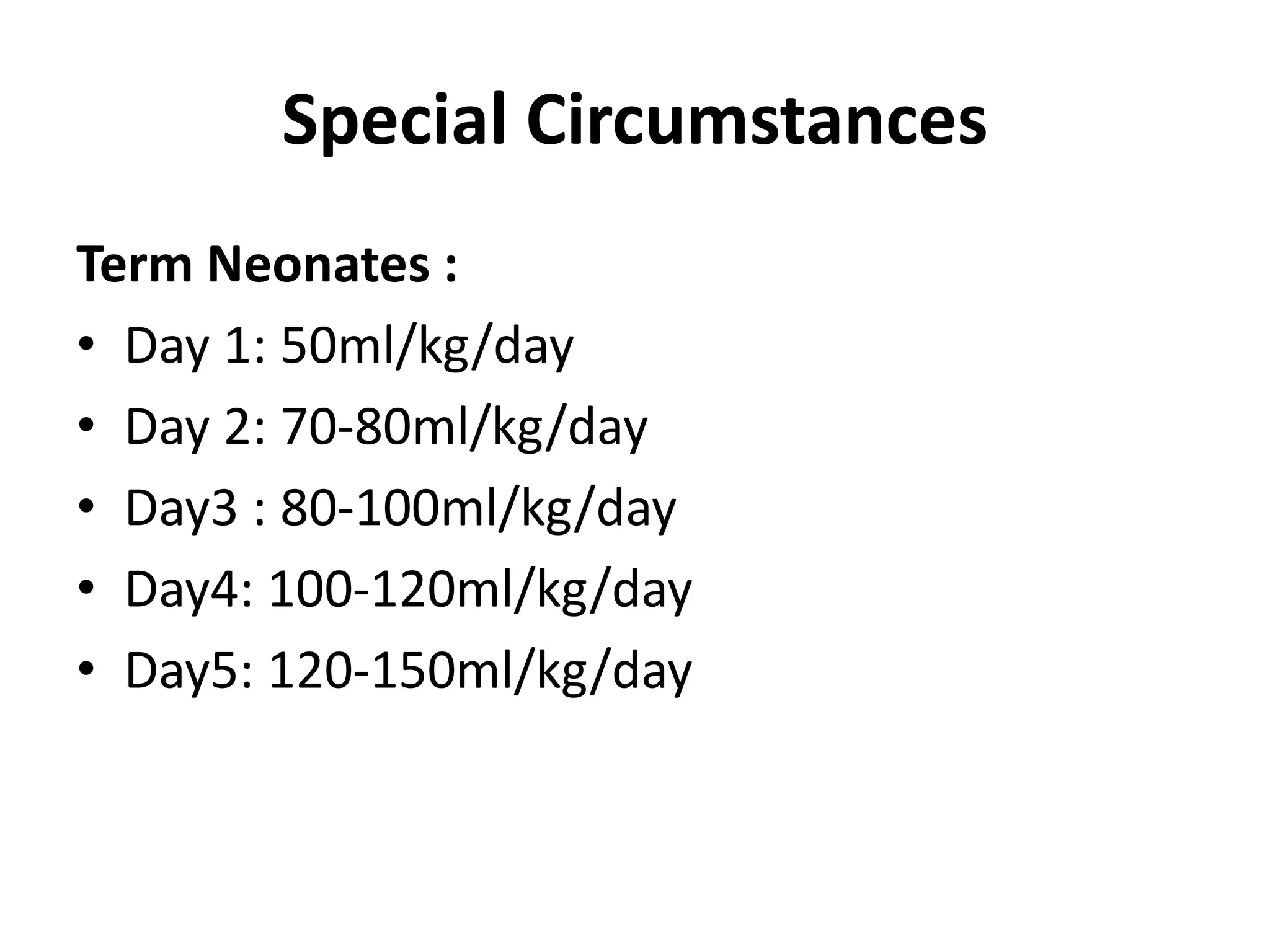
The document discusses the physiology and management of intravenous fluids in pediatrics, including types of IV fluids, their distribution in body compartments, and fluid replacement calculations. It explains maintenance and deficit fluid requirements, special circumstances in fluid management such as burns and neonates, and emphasizes the importance of monitoring electrolytes. Key points include the differences between crystalloids and colloids, the fluid distribution after administration, and guidelines for effective resuscitation phases.