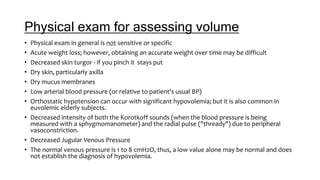
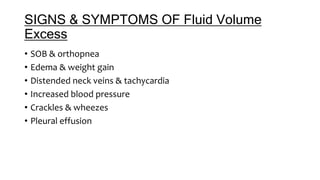
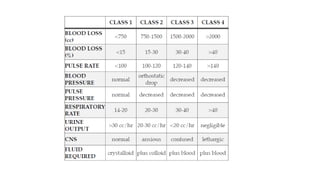
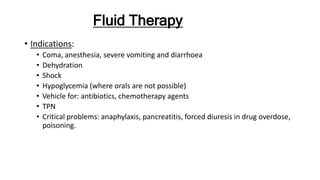
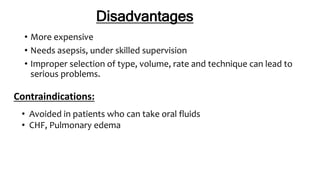
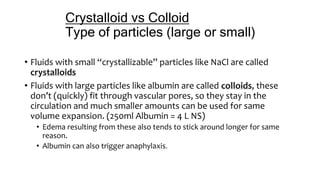
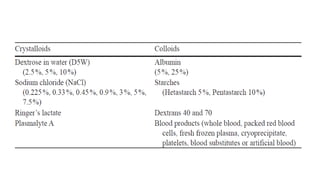
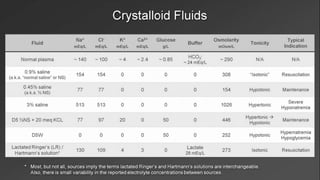
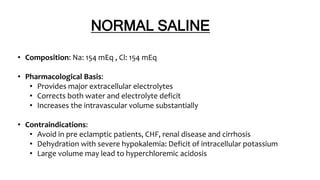
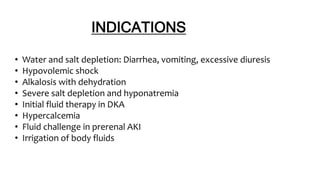
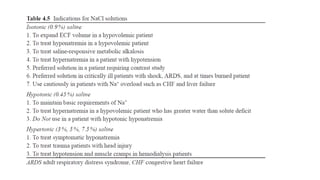
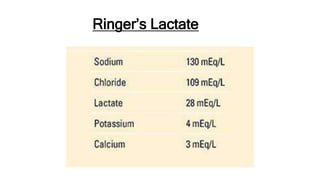
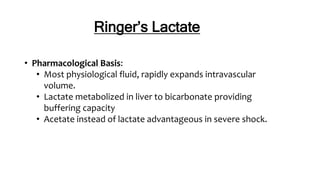
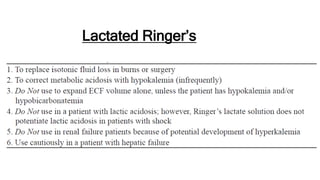
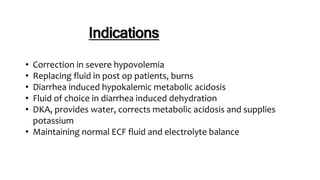
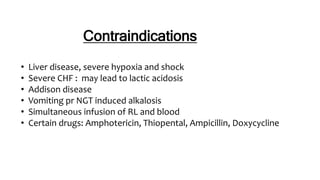
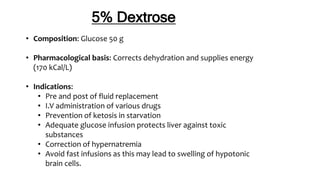
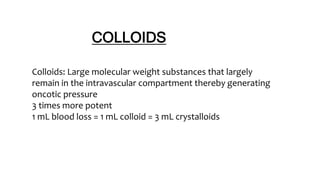
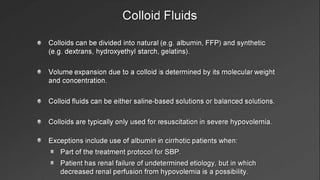
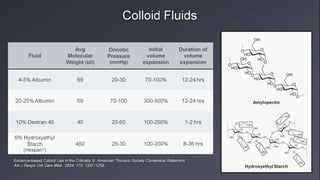
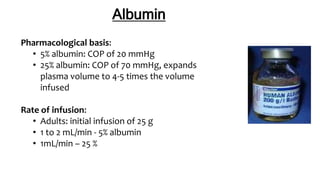
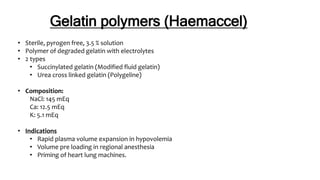
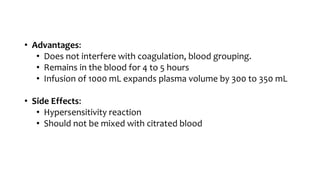
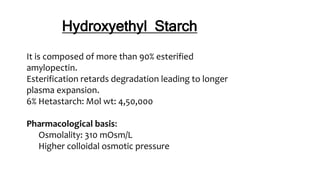
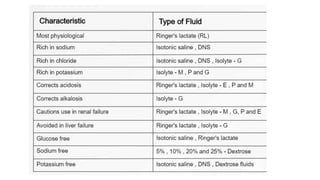
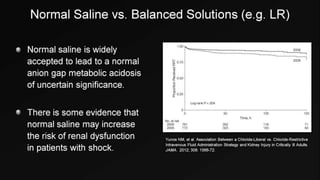
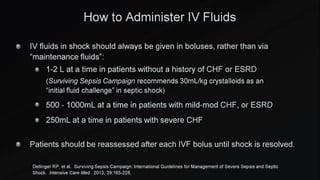
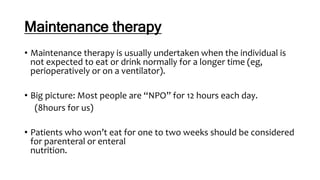
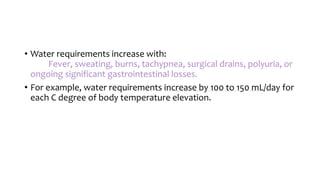
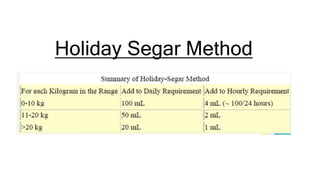
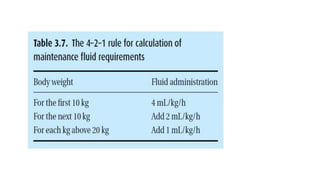
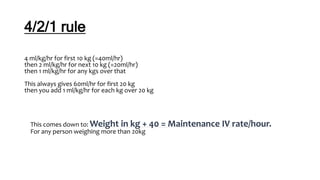
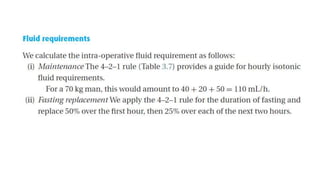
Physical exam findings of hypovolemia include decreased skin turgor, dry mucous membranes, orthostatic hypotension, and decreased jugular venous pressure. Signs of fluid overload include shortness of breath, edema, elevated jugular venous pressure, and crackles. Intravenous fluids are used for hydration, shock, and as vehicles for medications. Crystalloids like normal saline and lactated ringer's are used for initial resuscitation while colloids like albumin and hetastarch provide greater volume expansion over longer periods. Maintenance fluid rates are calculated based on weight and ongoing losses.