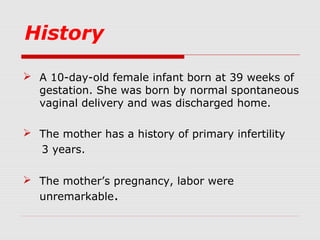
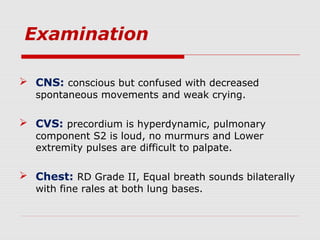
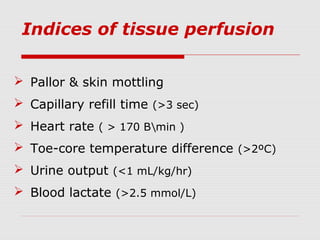
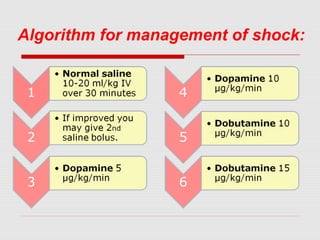
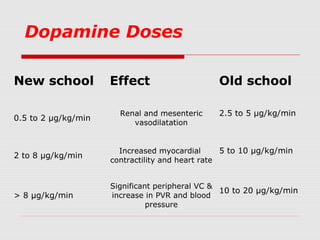
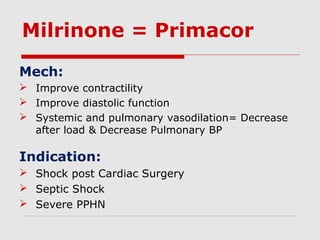
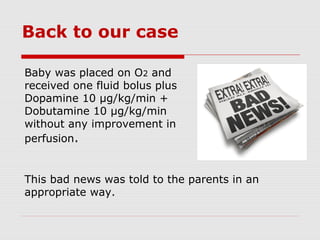
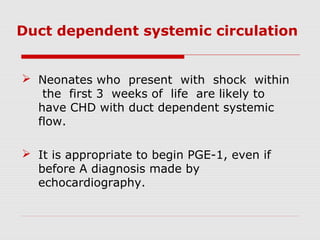
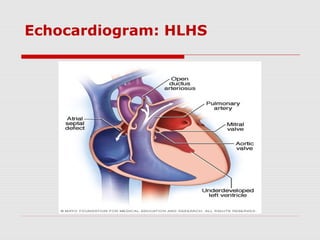
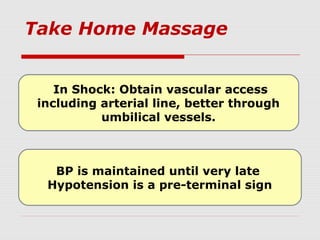
This document describes the case of a 10-day-old infant presenting with signs of shock including tachycardia, poor perfusion, and decreased urine output. Examinations revealed hepatomegaly and other signs suggestive of shock. Investigations showed metabolic acidosis and low blood sugar. The infant did not respond to initial fluid resuscitation and inotropic support. Echocardiogram revealed hypoplastic left heart syndrome. Prostaglandin E1 was started and the infant responded, confirming duct-dependent systemic circulation. The case highlights the importance of early recognition and management of neonatal shock.