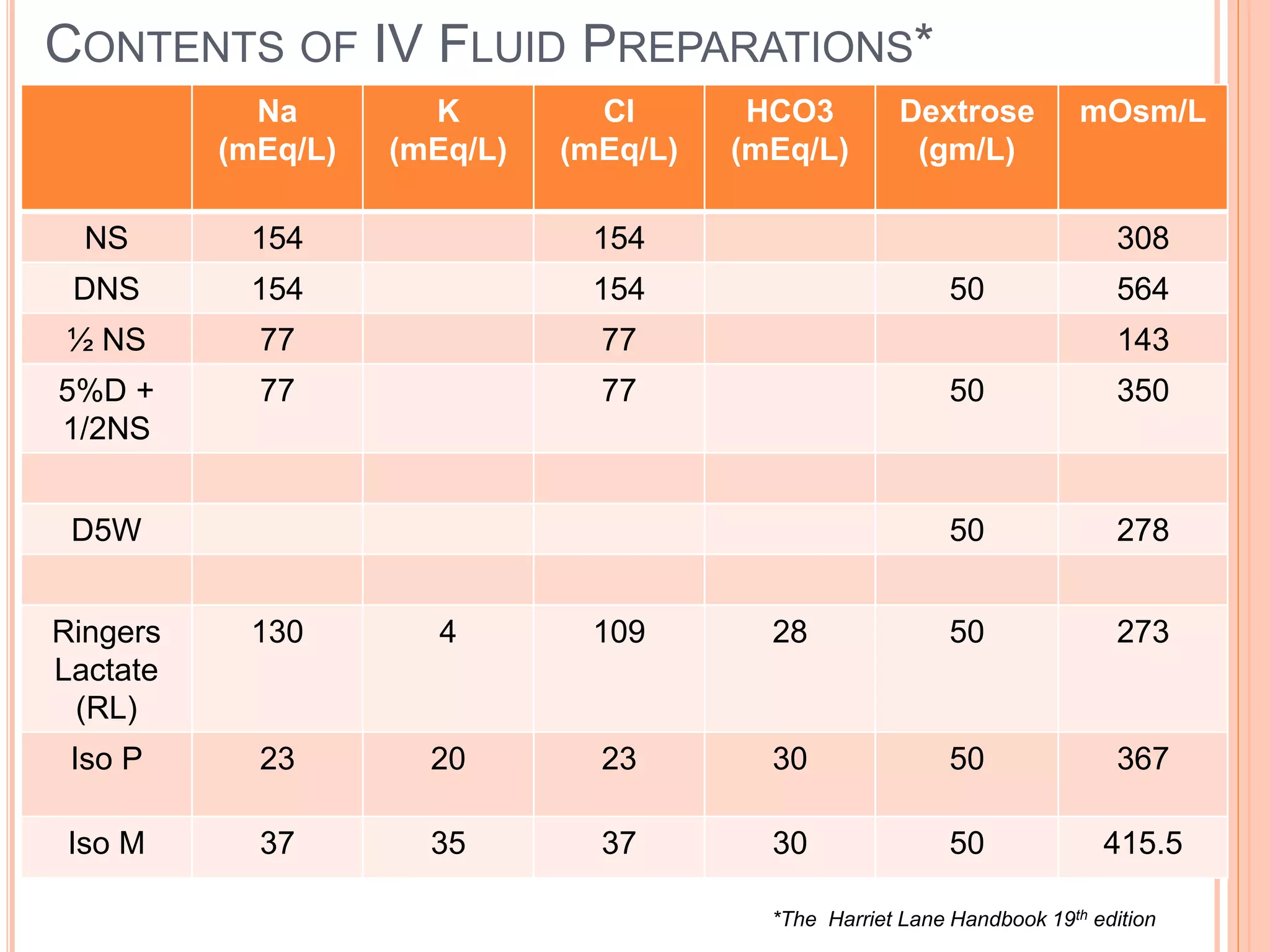
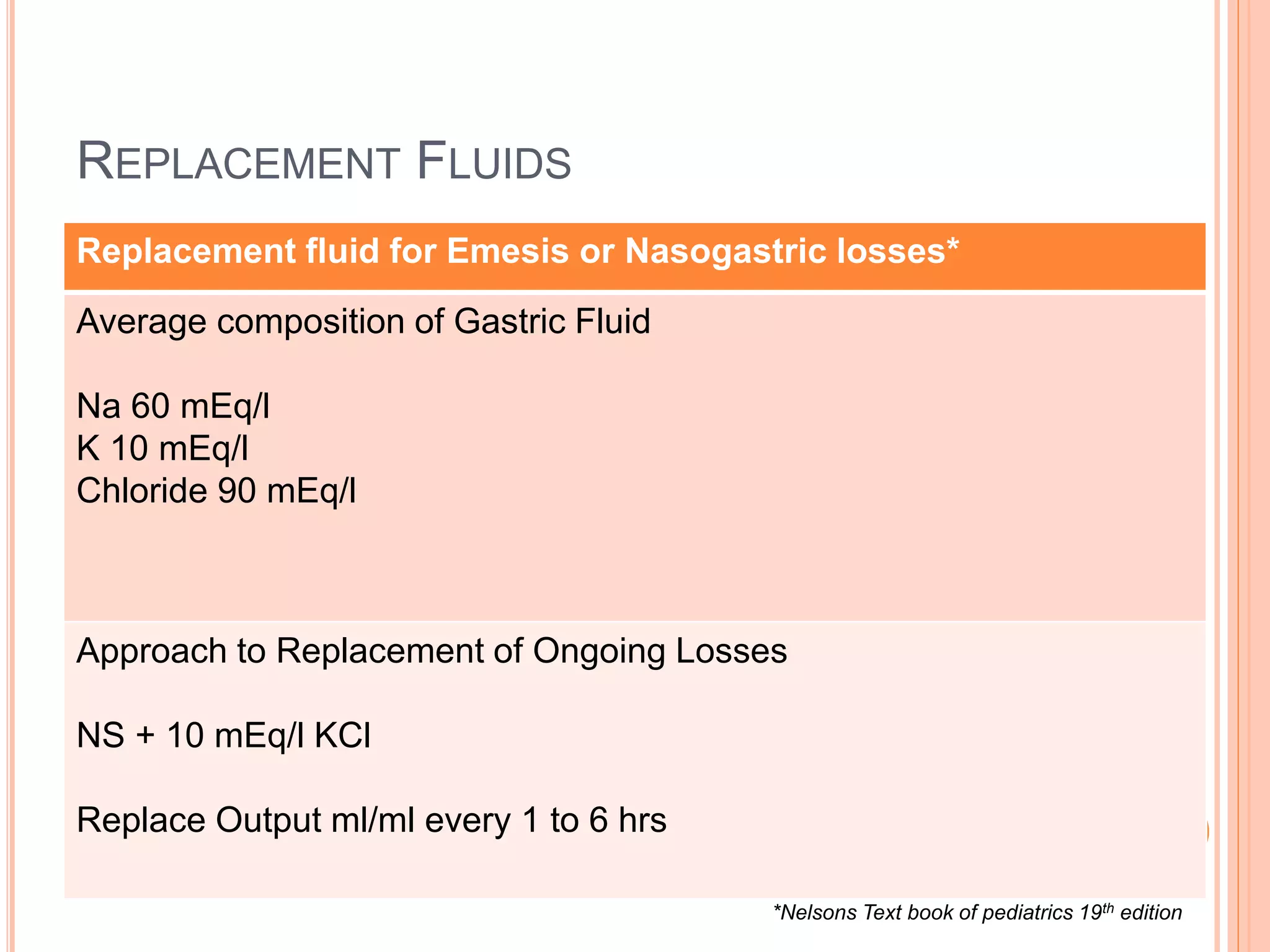
This document discusses maintenance and replacement fluid therapy in children. It begins by outlining the objectives of understanding the differences in pediatric physiology and the goals of maintenance fluid therapy. It then covers topics like the vulnerability of infants, the distribution of body water, electrolyte concentrations, commonly used IV fluids, and calculating fluid requirements using the 4-2-1 rule. The document emphasizes the importance of monitoring weight, urine output, and serum electrolytes when administering fluids. It also provides guidance on choosing appropriate replacement fluids for issues like diarrhea, vomiting, and altered renal output.









![KEY LEARNING POINT*
Sodium is the Principle electrolyte in ECF
[140mEq/L (+/- 5)]
Potassium is the Principle electrolyte in ICF
[150mEq/L (+/- 5)]
*IAP text book of Pediatrics 5th edition](https://image.slidesharecdn.com/maintainancereplacementfluidtherapy-141226142052-conversion-gate02/75/Maintainance-replacement-fluid-therapy-pediatrics-AG-12-2048.jpg)