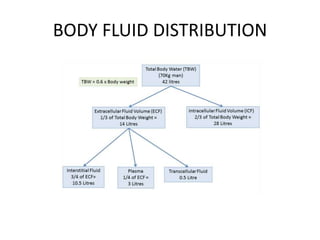
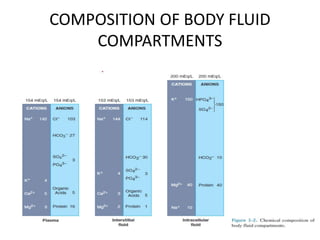
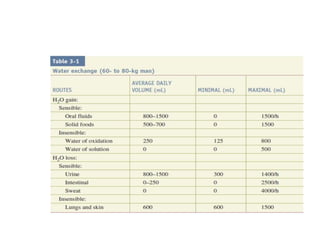
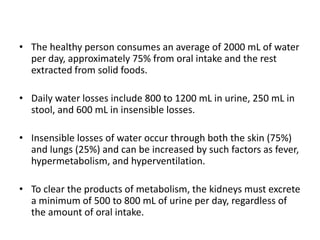
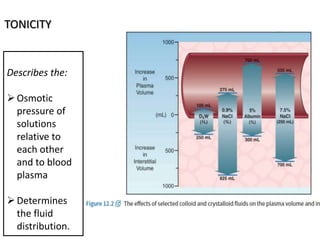
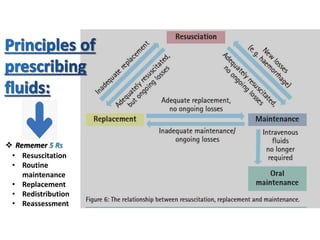
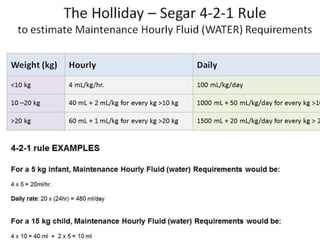
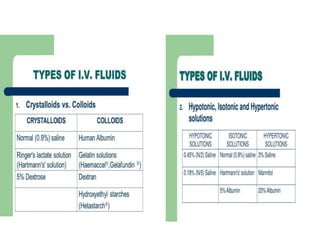
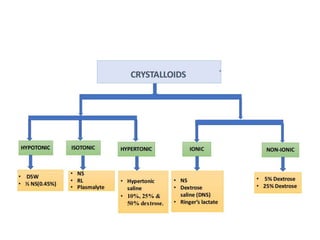
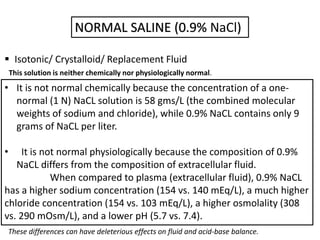
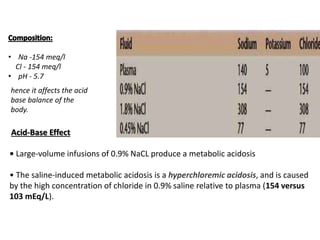
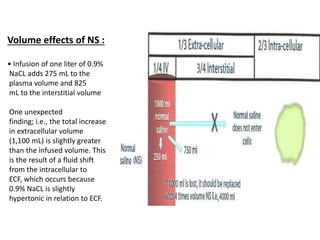
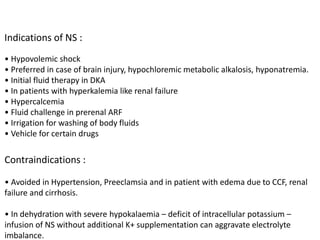
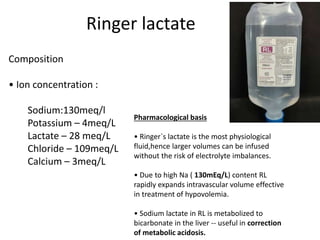
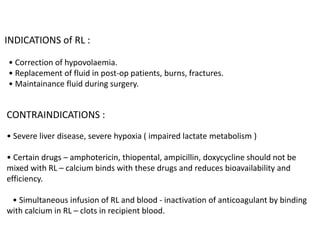
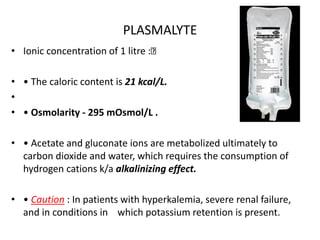
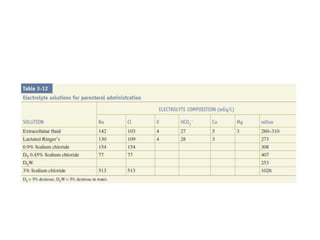
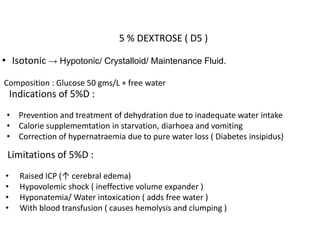
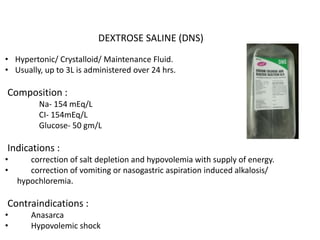
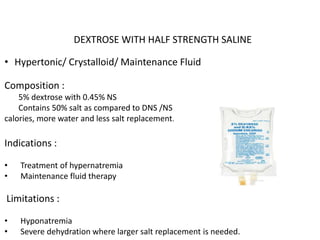
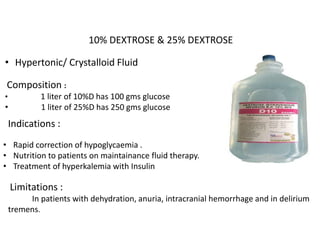
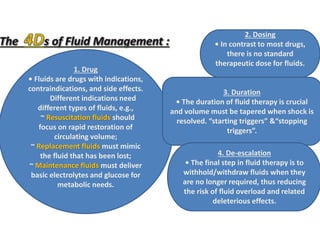
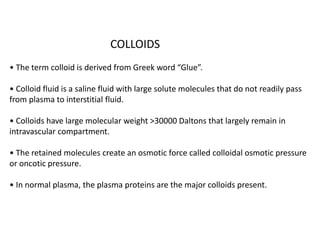
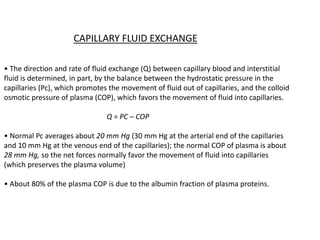
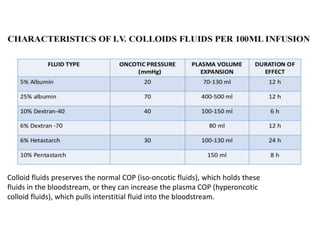
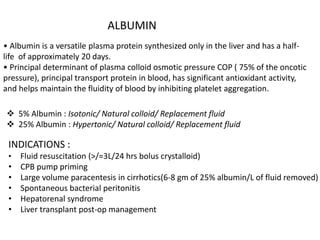
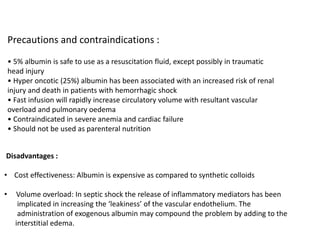
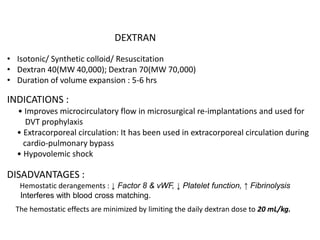
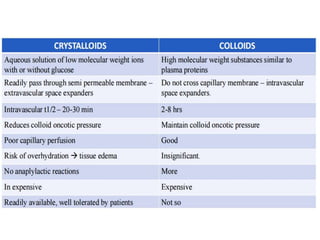
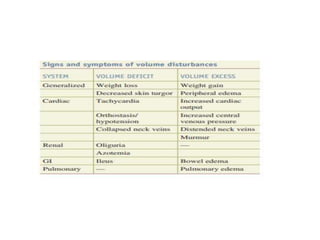
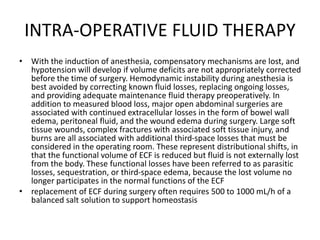
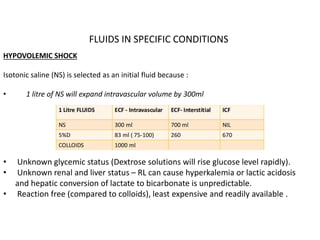
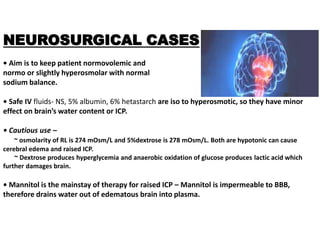
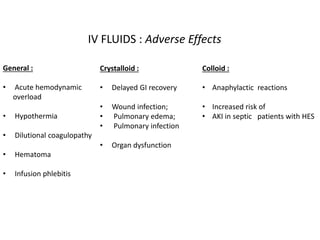
This document discusses fluid management in surgery. It begins by introducing the importance of fluid and electrolyte balance for maintaining homeostasis. Different types of fluids are indicated for various purposes like rapid resuscitation, total parenteral nutrition, and fluid maintenance. Common fluids discussed include normal saline, Ringer's lactate, plasmalyte, dextrose solutions, and dextrose saline. The document explains the composition, indications, advantages/limitations of each fluid. It also covers fluid distribution in the body, osmolality, tonicity, and the role of colloids in fluid balance.