intraoperative management in anesthesia and surgery. Adequate fluid administration ensures maintenance of intravascular volume, tissue perfusion, and organ oxygen delivery, while avoiding the morbidity associated with both hypovolemia and fluid overload.
Perioperative fluid balance is influenced by anesthetic technique, surgical trauma, patient comorbidities, and the dynamic changes in vascular permeability and redistribution of body water. Thus, fluid therapy must be individualized rather than formulaic.
---
Historical Background
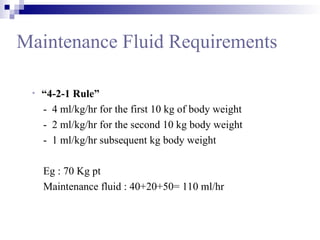
Earlier, fluid replacement was based on the “4-2-1 rule” and the “third-space loss” concept. Recent evidence, however, has shifted practice towards restrictive or goal-directed therapy. Advances in monitoring (pulse contour analysis, esophageal Doppler, dynamic preload indices) have refined how intraoperative fluids are guided.
---
Physiology of Fluid Balance
The human body contains approximately 60% of body weight as water.
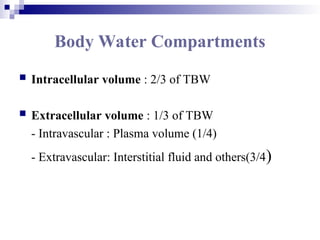
Intracellular fluid (ICF): 2/3 of total body water.
Extracellular fluid (ECF): 1/3, of which plasma is 1/4 and interstitial fluid is 3/4.
Fluid movement between compartments depends on Starling forces:
Hydrostatic pressure.
Oncotic pressure (albumin major contributor).
Capillary permeability.