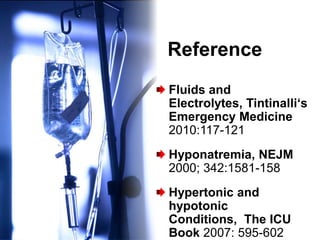
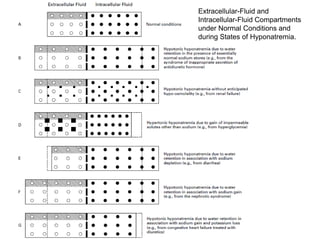
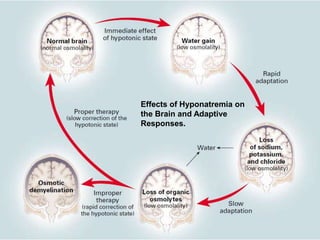
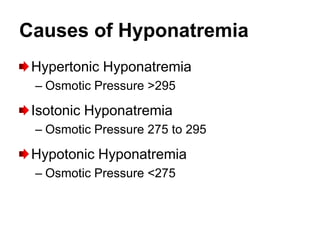
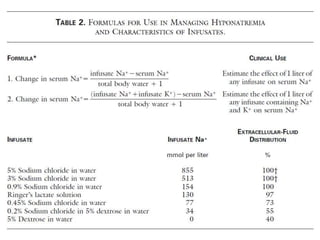
This document discusses hyponatremia, defined as a sodium level below 135 mEq/L. It describes the fluid compartments in the body under normal conditions and with hyponatremia. Causes of hyponatremia include excessive water intake, syndrome of inappropriate antidiuretic hormone secretion, and liver or kidney failure. Symptoms range from nausea and vomiting to seizures and coma. Severe hyponatremia below 115 mEq/L may warrant emergency treatment to correct the sodium level by no more than 1 mEq/L/hour. The document provides extensive details on the causes, diagnosis, and treatment of hyponatremia.
![Hyponatremia
[Na] < 135 mEq/L](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-1-320.jpg)
![Clinical Signs of Hyponatrema
Nausea, vomiting, anorexia, muscle
cramps, confusion, and lethargy, and
culminate ultimately in seizures and coma.
Seizures are quite likely at [Na+] of 113
mEq/L or less.](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-4-320.jpg)
![Hypotonic hyponatremia (Posm <275)
Hypovolemic Euvolemic
– Renal urine [Na+] usually > 20 mEq/L
• Diuretic use – SIADH
• Salt-wasting nephropathy (renal tubular – Hypothyroidism (possible increased ADH
acidosis, chronic renal failure, interstitial
nephritis)
or deceased glomerular filtration rate)
• Osmotic diuresis – Pain, stress, nausea, psychosis
(glucose, urea, mannitol, hyperproteinemia) (stimulates ADH)
– Drugs:
• Mineralocorticoid (aldosterone) deficiency ADH, nicotine, sulfonylureas, morphine,
– Extrarenal barbiturates, NSAIDs, acetaminophen,
• Volume replacement with hypotonic fluids carbamazepine, phenothiazines, tricyclic
• GI loss (vomiting, diarrhea, fistula, tube antidepressants, colchicine, clofibrate,
suction) cyclophosphamide, isoproterenol,
• Third-space loss (e.g., burns, hemorrhagic tolbutamide, vincristine, monoamine
pancreatitis, peritonitis) oxidase inhibitor
Hypervolemic – Water intoxication
– Urinary [Na+] >20 mEq/L – Glucocorticoid deficiency
• Renal failure (inability to excrete free water) – Positive pressure ventilation
– Urinary [Na+] <20 mEq/L – Porphyria
• Congestive heart failure – Essential (reset osmostat or sick cell
• Nephrotic syndrome syndrome—usually in the elderly)
• Cirrhosis](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-8-320.jpg)
![Diagnostic Criteria for Syndrome
of Inappropriate Secretion of ADH
Hypotonic hyponatremia
Inappropriately elevated urine osmolality
(usually >200 mOsm/kg)
Elevated urine [Na+] (typically > 20 mEq/L)
Clinical euvolemia
Normal adrenal, renal, cardiac, hepatic, and
thyroid function
Correctable with water restriction](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-9-320.jpg)
![Total Body [Na+] Deficit
= (desired plasma [Na+]-measured plasma [Na+])
×TBW](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-11-320.jpg)
![Emergency Treatment of Severe
Hyponatremia
Although specific or general treatment of
hyponatremia for the condition discussed may be
initiated in the ED, there is generally little
urgency to address the hyponatremia
immediately when [Na+] is 120 mEq/L.
If hyponatremia is severe (<115 mEq/L or when
the patient is symptomatic), treatment should be
initiated.](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-12-320.jpg)
![Emergency Treatment of Severe
Hyponatremia
Situations that warrant consideration of emergent
treatment are hypovolemic patients and patients
in extremis, (e.g., mental status changes or
coma). In hypovolemic patients, the [Na+] deficit
should be calculated and replaced with normal
saline solution.
Urine electrolytes are useful only before
beginning treatment and therefore should be
collected in the ED.
The rise in [Na+] should be no greater than 0.5
to 1.0 mEq/L per hour.](https://image.slidesharecdn.com/hyponatremia-130407233646-phpapp01/85/Hyponatremia-13-320.jpg)