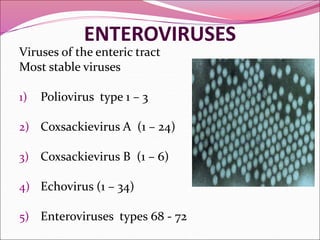
This document discusses enteroviruses, which are small RNA viruses that infect the gastrointestinal or respiratory tract. It covers the classification, properties, pathogenesis, clinical features, diagnosis and prevention of several enteroviruses including poliovirus, coxsackievirus, echovirus, and rhinovirus. Key points include that poliovirus can cause paralysis, there are live and inactivated polio vaccines, and global efforts aim to eradicate poliovirus transmission. Coxsackievirus A can cause herpangina while B is associated with myocarditis. Echoviruses commonly cause asymptomatic infections or rash. Rhinoviruses are a common cause of the common cold.