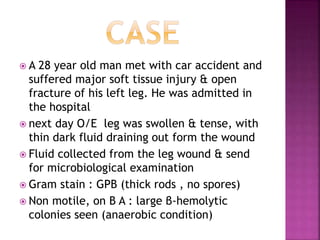
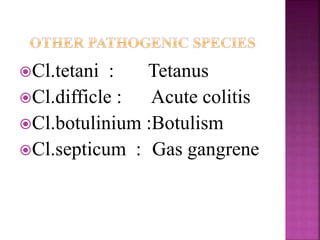
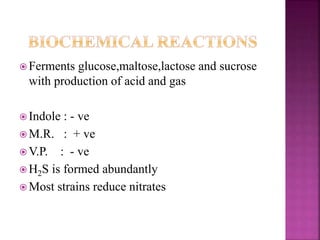
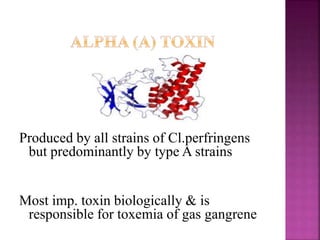
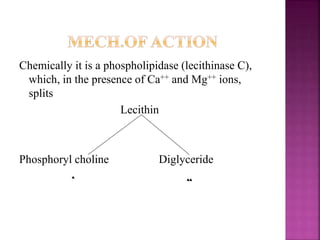
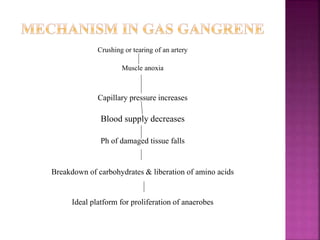
A man was admitted to the hospital with a major soft tissue injury and open leg fracture from a car accident. His leg wound drained a thin, dark fluid. Microbiological examination of the fluid found gram-positive thick rods without spores on gram stain (Clostridium perfringens). C. perfringens is a pathogenic, spore-forming, anaerobic bacterium that can cause gas gangrene, food poisoning, and necrotizing enteritis by producing various toxins. It is commonly found in the intestines but can cause disease when introduced into deep tissue wounds.