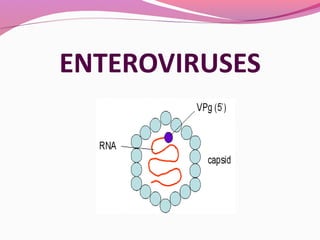
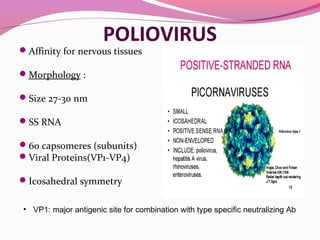
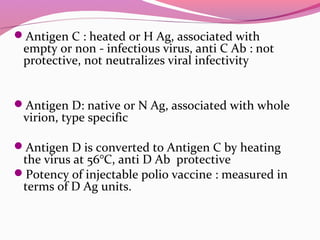
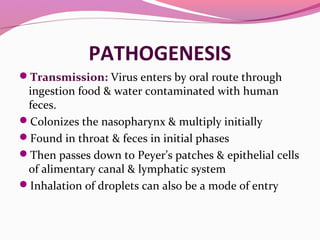
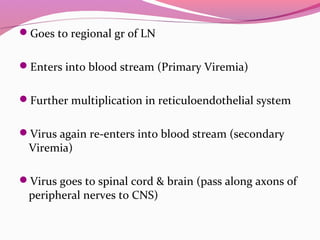
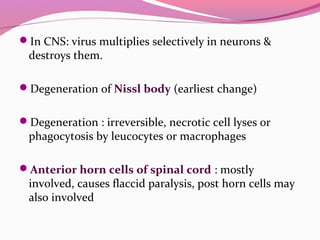
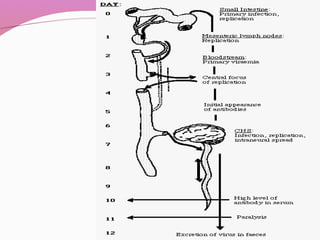
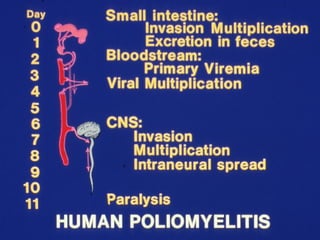
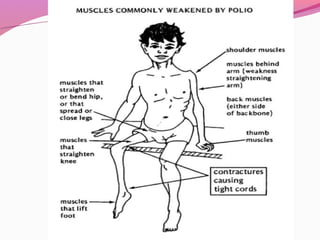
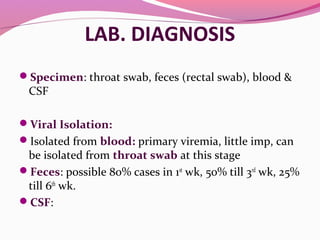
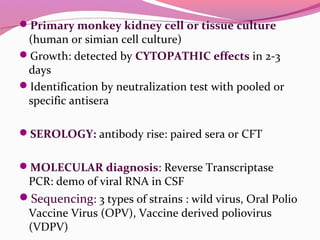
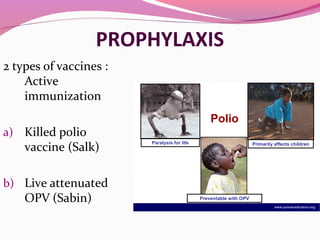
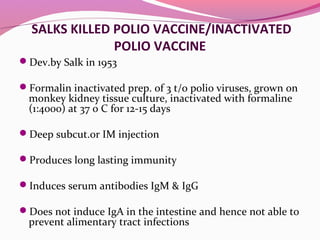
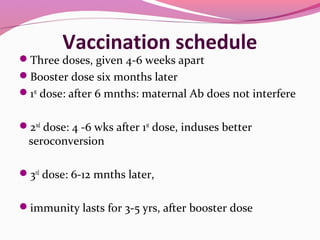
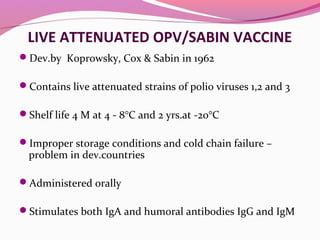
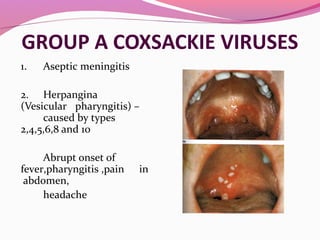
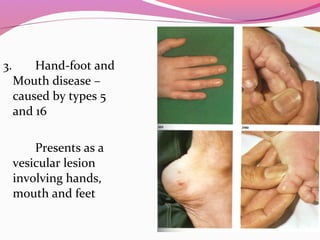
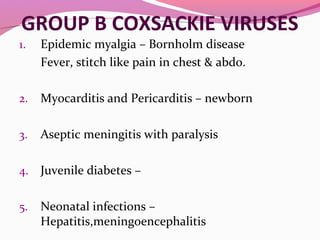
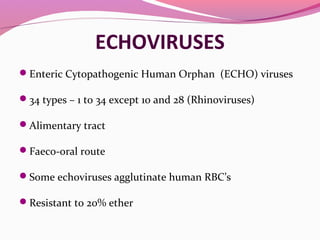
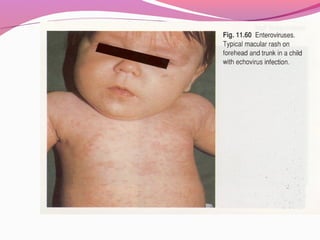
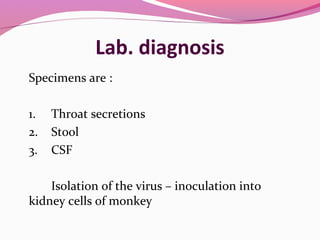
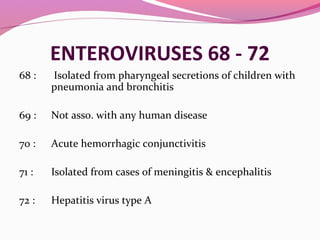
This document provides information on picornaviruses including enteroviruses. It discusses the classification, properties, laboratory diagnosis and clinical features of important enteroviruses such as poliovirus, coxsackievirus, echovirus and newer enteroviruses 68-72. Poliovirus is described in more detail including its morphology, antigenic properties, pathogenesis of paralytic poliomyelitis, and prevention through polio vaccines.