This document summarizes a talk given on device checks and outcomes, device interrogation, magnet operation for ICDs and pacemakers, and CareLink Express status in Western Australia. Some key points:
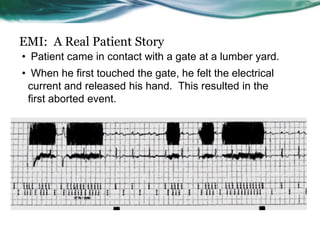
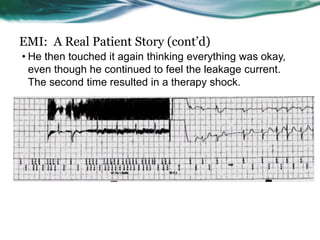
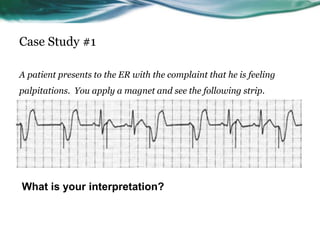
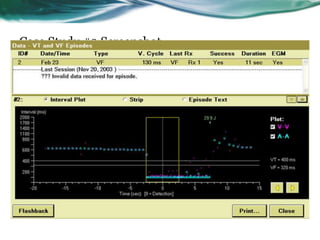
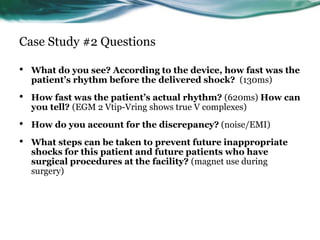
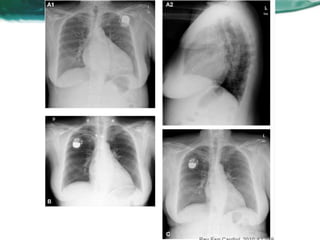
- Common reasons for device checks in the ED include syncope, palpitations, device beeping, shocks, and patient feeling unwell. Device interrogation and magnet operation were demonstrated.
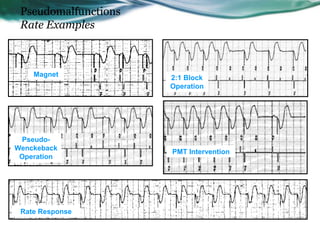
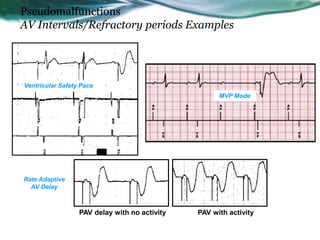
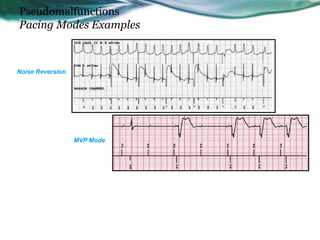
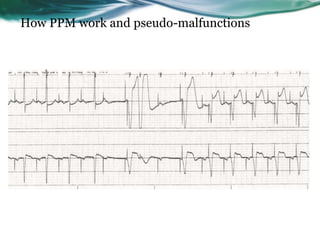
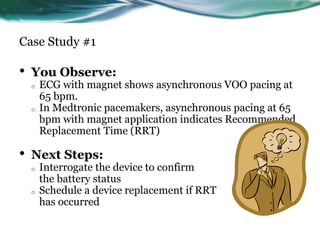
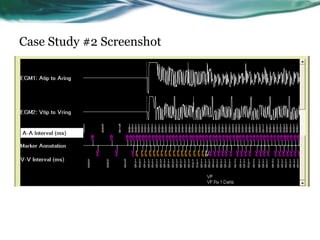
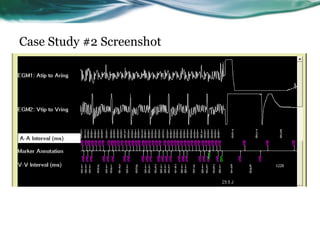
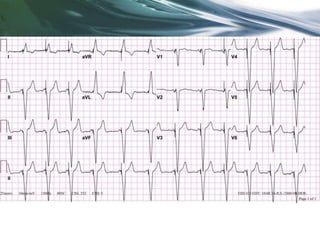
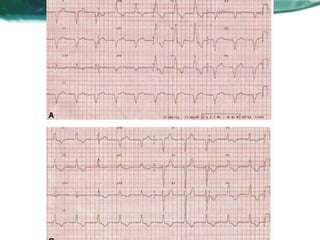
- Pseudomalfunctions are ECG findings that appear abnormal but represent normal device function, like rate changes from magnet use or device algorithms.
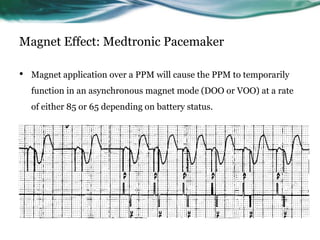
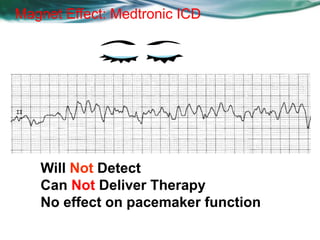
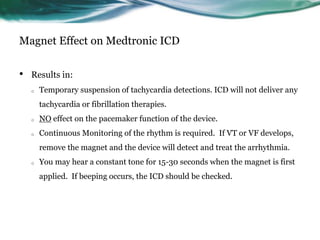
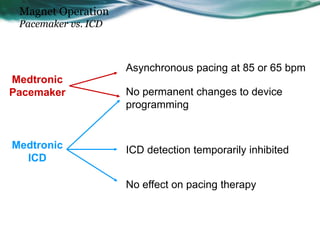
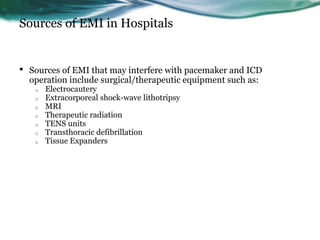
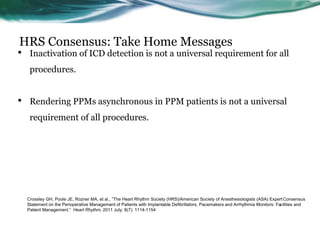
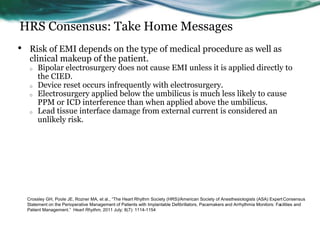
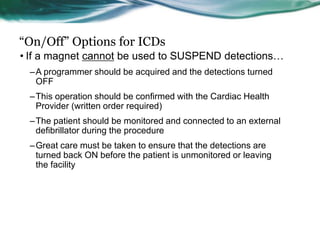
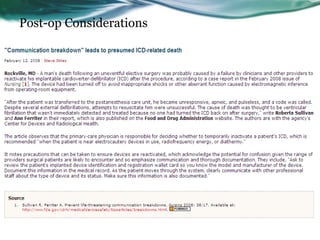
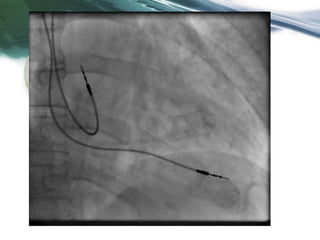
- Magnet application sets pacemakers to asynchronous mode and inhibits ICD therapy temporarily.
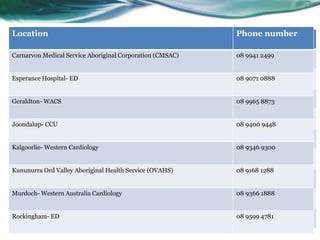
- CareLink Express allows remote device interrogation and is available at various hospitals and clinics in