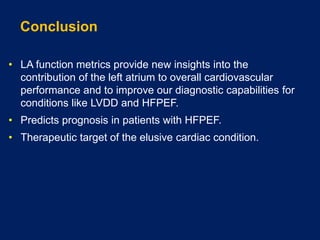
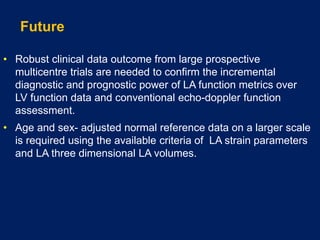
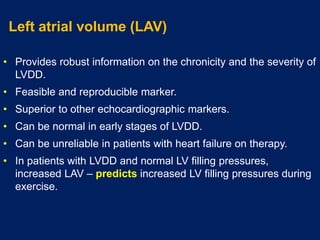
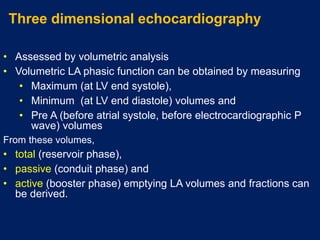
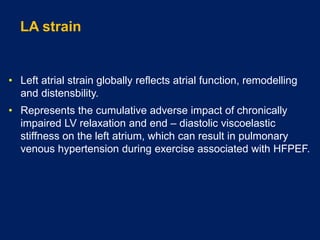
This document discusses the importance of assessing left atrial function using echocardiography. Left atrial volume and strain are superior to other echocardiographic markers for diagnosing left ventricular diastolic dysfunction. Left atrial reservoir strain in particular shows high specificity but relative low sensitivity for diagnosing heart failure with preserved ejection fraction compared to invasive exercise assessment. More research is still needed to establish robust clinical data on using left atrial function metrics for diagnosis.


![Left atrial structure and function in HFPEF
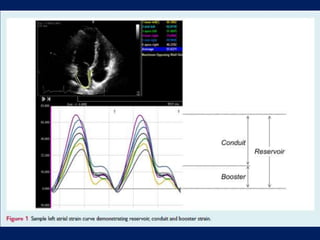
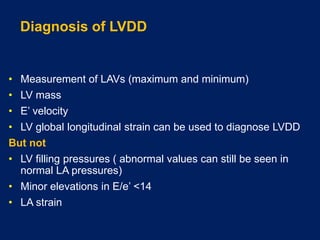
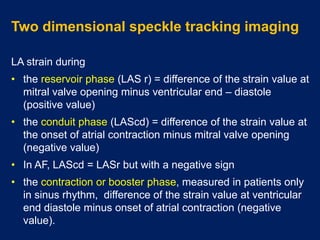
• Accuracy of LA strain in patients with unexplained dyspnoea,
where the diagnosis of HFPEF was definitely confirmed or
refuted using maximal effort invasive exercise assessment.
• LA reservoir strain was highly feasible and demonstrated net
classification improvement when LA reservoir strain was
added to recommended echocardiographic parameters used
to diagnose HFPEF.
• LA stiffness index still added further improvement.
Reddy YN, Obokata M, Egbe A, Yang JH, Pislaru S, Lin G, Carter R, Borlaug BA. Left atrial strain and compliance
in the diagnostic evaluation of heart failure with preserved ejection fraction. Eur J Heart Fail 2019 Mar 28.
doi: 10.1002/ejhf-1464 [Epub ahead of print].](https://image.slidesharecdn.com/leftatrialfunction-191013173159/85/Left-atrial-function-11-320.jpg)