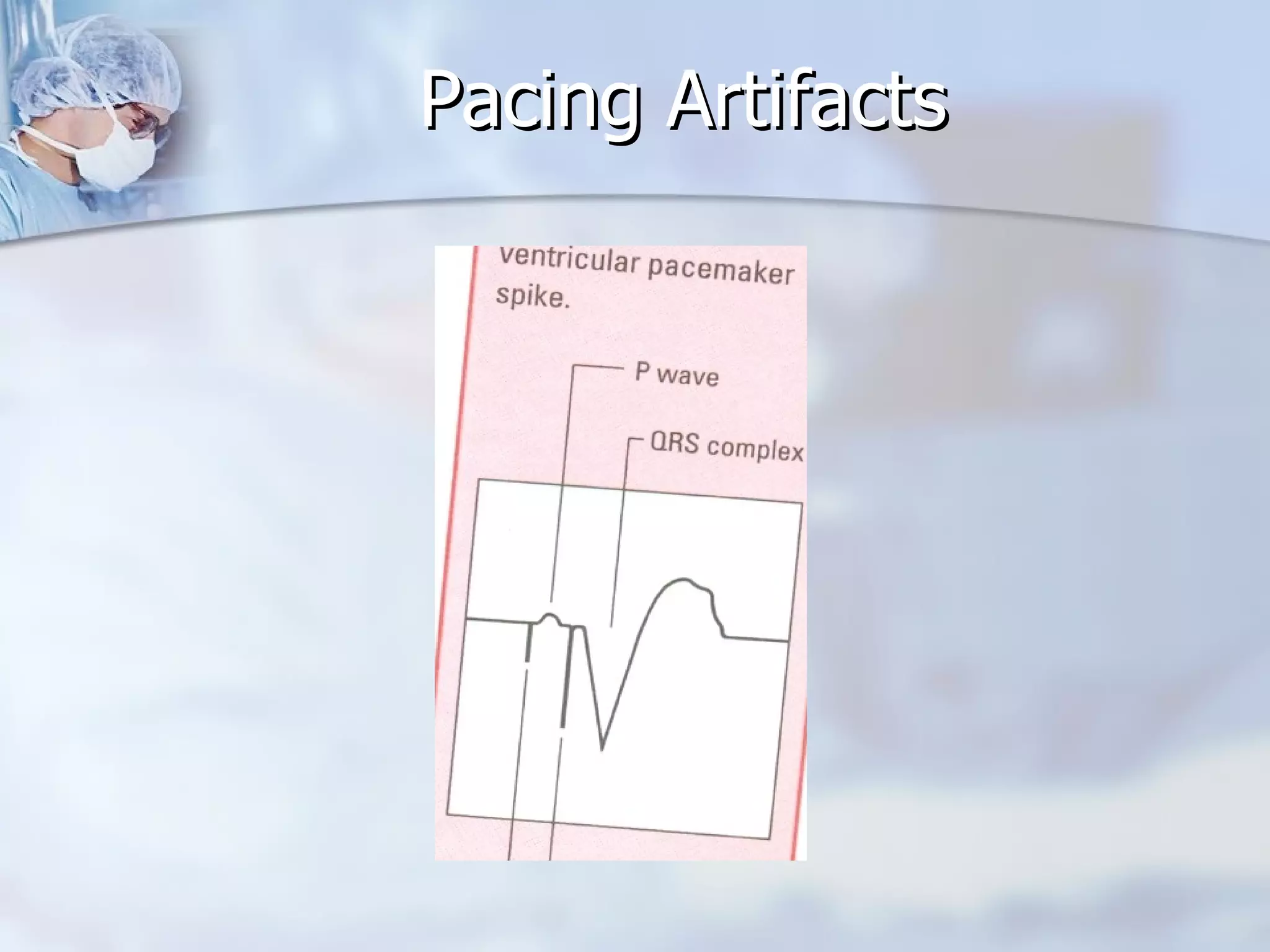
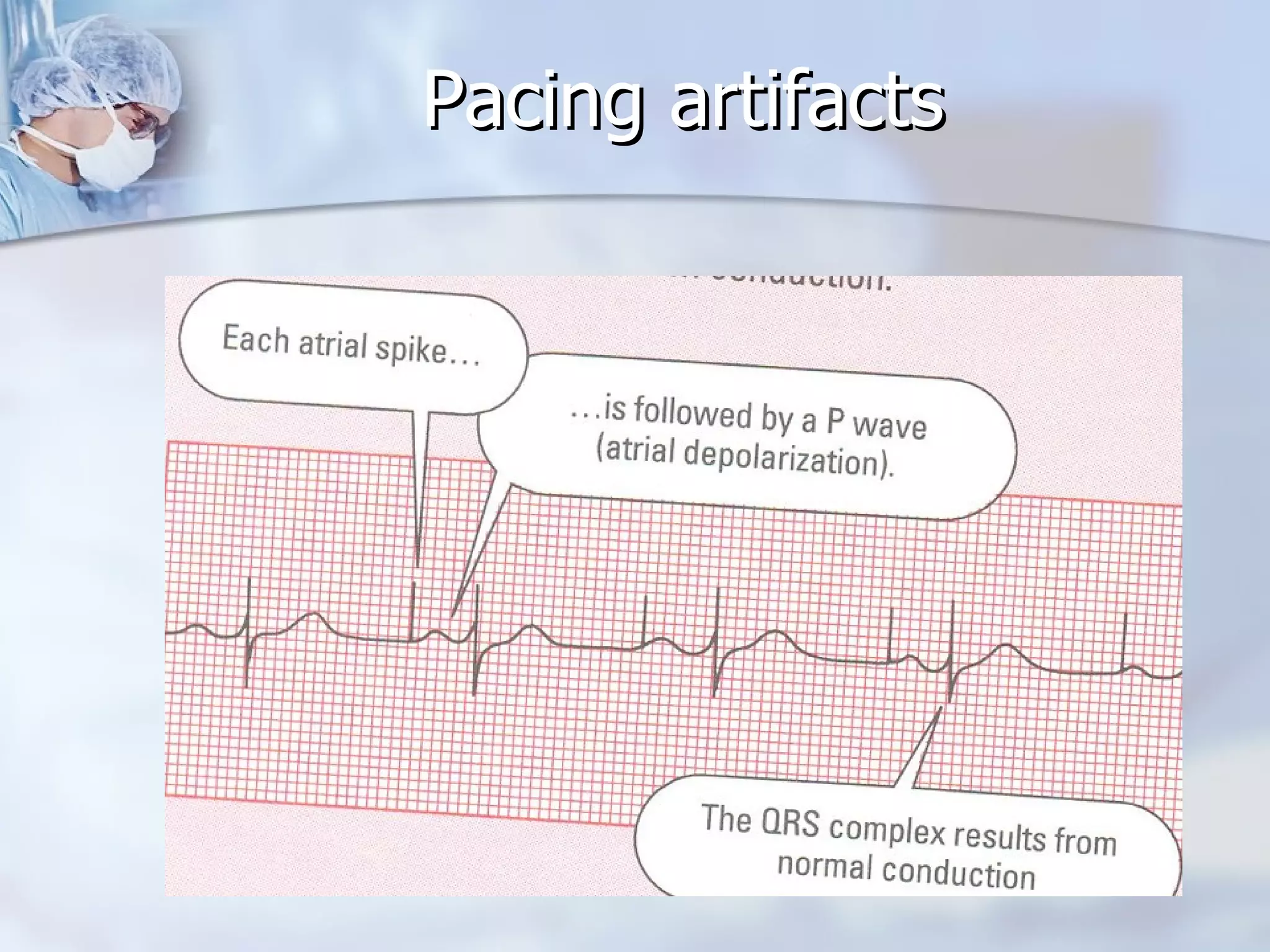
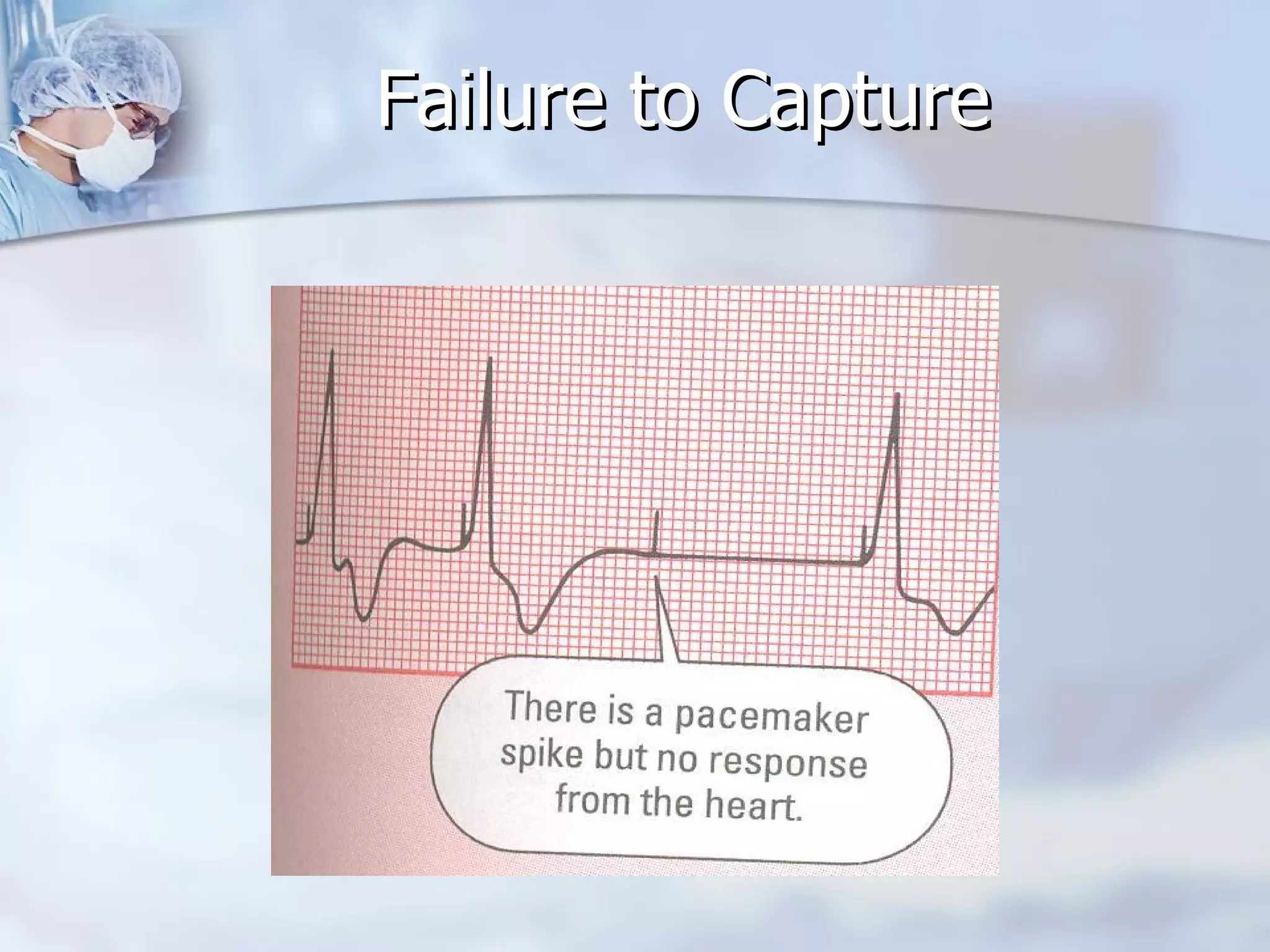
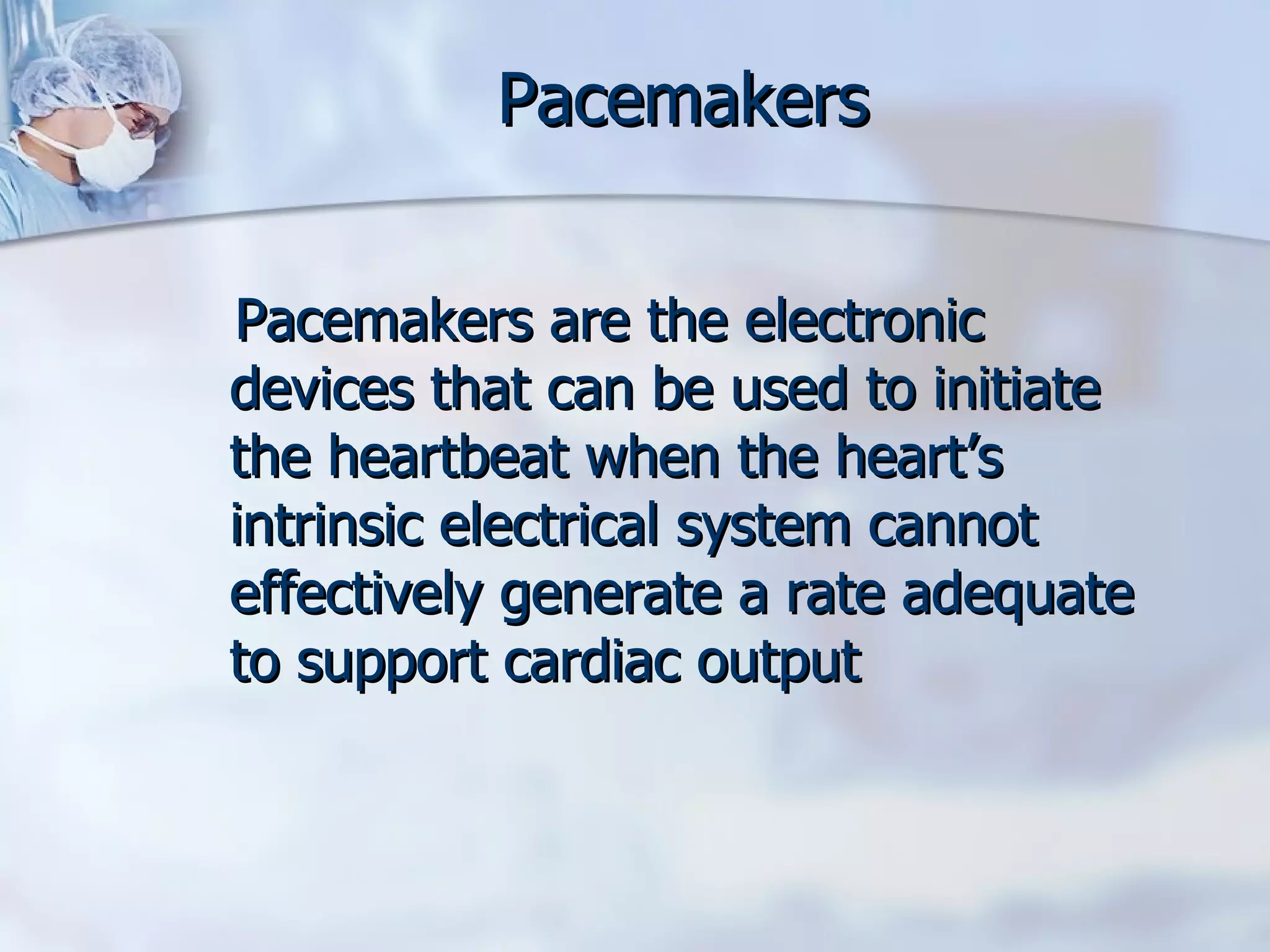
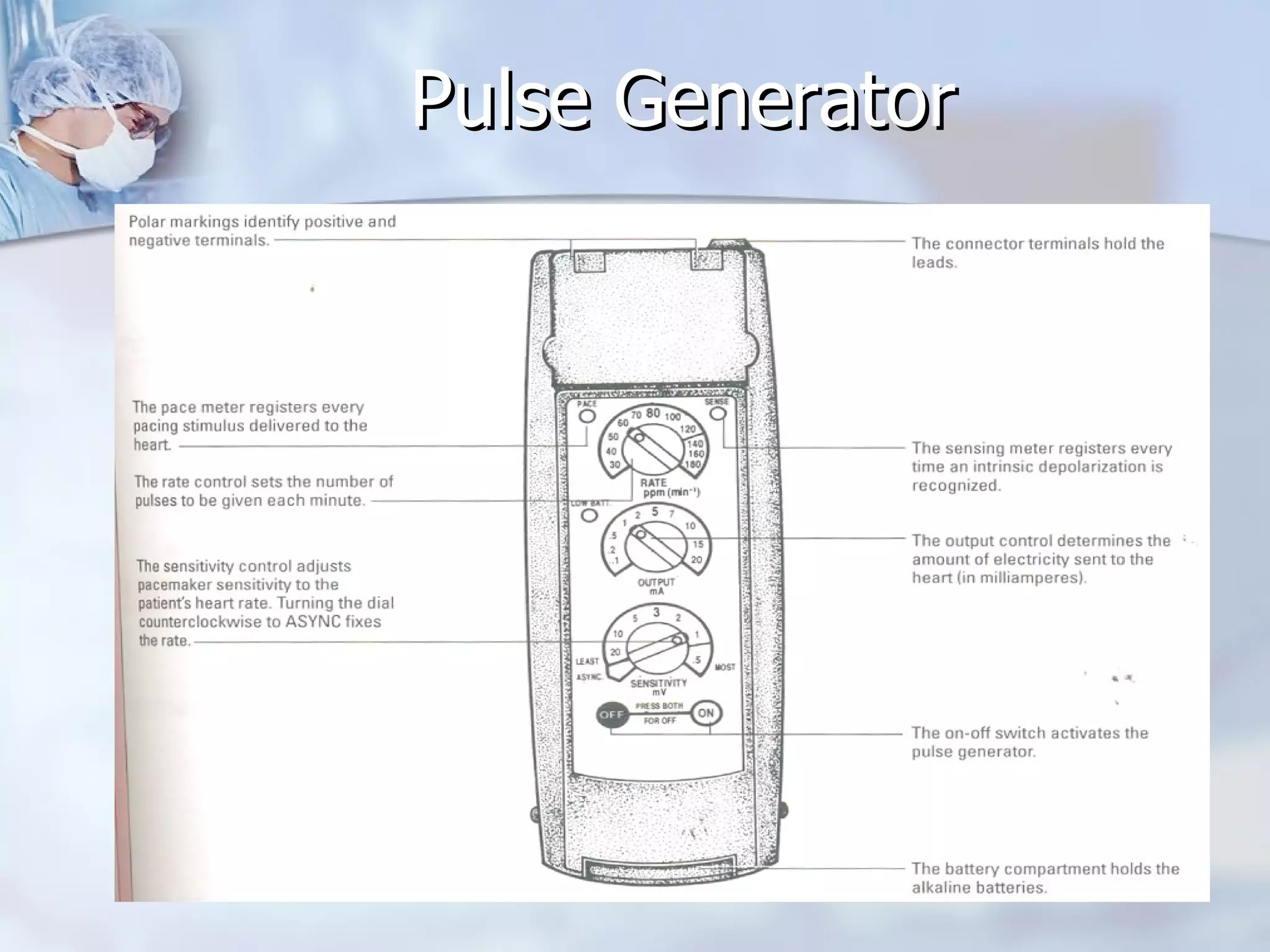
Pacemakers are electronic devices that can be used to initiate a heartbeat when the heart's intrinsic electrical system cannot effectively generate an adequate heart rate. There are temporary pacemakers, which are used until the underlying condition resolves, and permanent pacemakers. A pacemaker system consists of a pulse generator and pacing leads. The pulse generator delivers electrical pulses through the leads to stimulate the heart. Pacemakers can pace one or both chambers of the heart and are programmed with settings for rate, output, and sensitivity. Nurses monitor for pacemaker function and complications and educate patients on pacemaker care.


![OUTPUT It is the amount of electrical current (measured in milliamperes [mA]) that is delivered to the heart to initiate depolarization. The point at which depolarization occurs is termed threshold and is indicated by a myocardial response to the pacing stimulus (capture)](https://image.slidesharecdn.com/temporarypacemakerslides-13001801149919-phpapp02/75/Temporary-Pacemaker-Slides-24-2048.jpg)