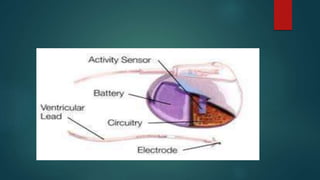
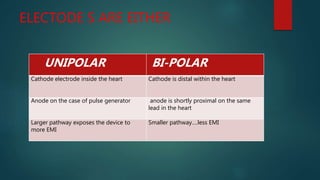
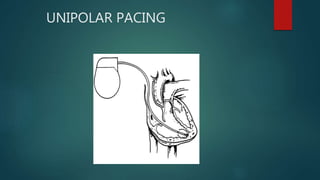
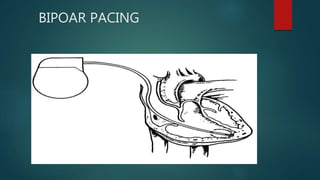
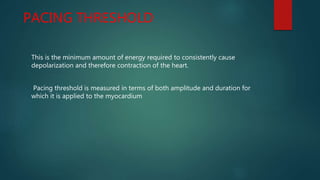
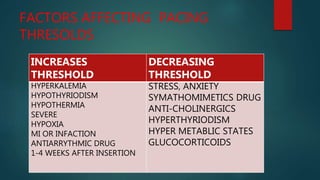
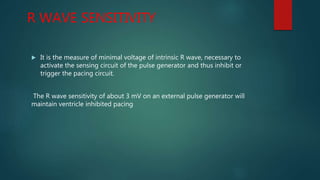
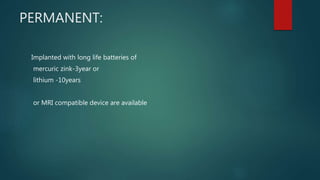
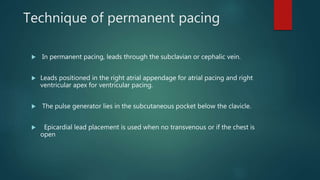
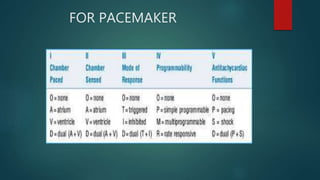
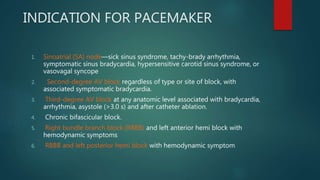
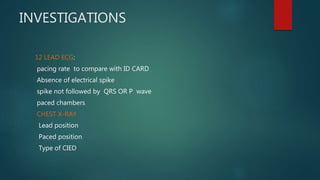
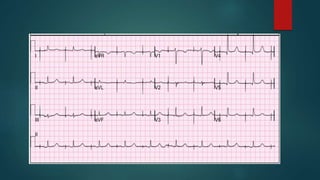
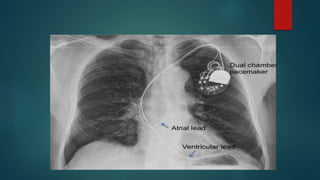
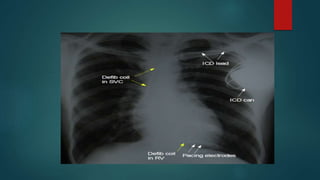
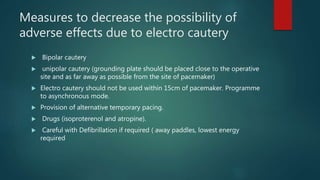
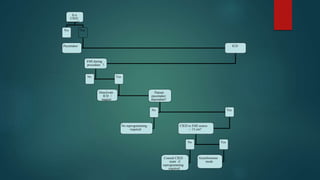
The document discusses cardiac pacemakers and implantable cardioverter defibrillators (ICDs). It covers the history, components, functions, types of pacing modes, indications for use, problems that can occur, and considerations for anesthetic management of patients with these devices. The key points are that pacemakers are used to treat bradycardia while ICDs treat tachycardia/fibrillation. Care must be taken with electromagnetic interference and device function needs to be considered for any procedures.