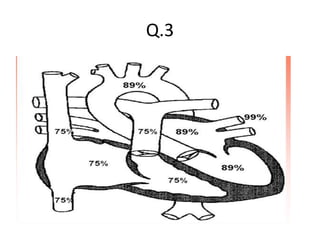
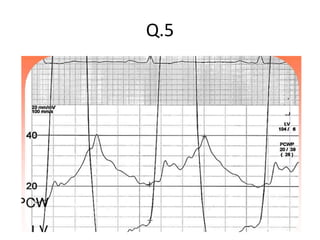
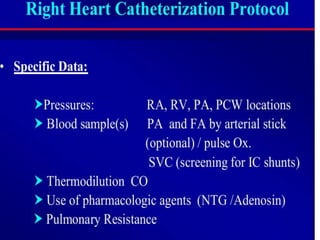
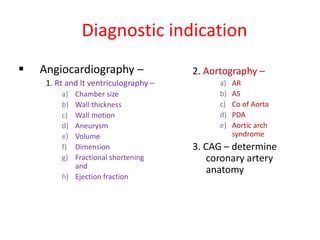
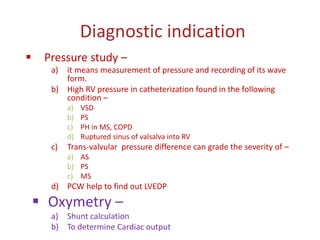
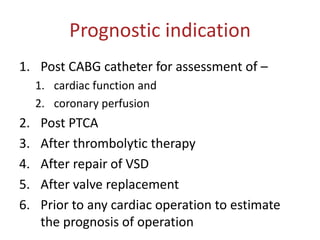
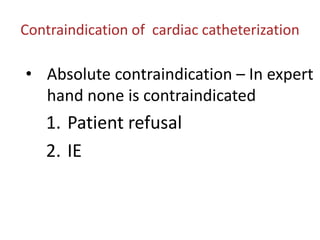
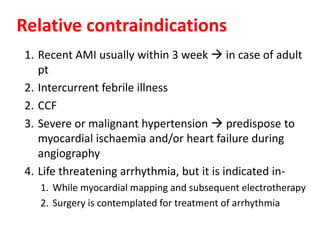
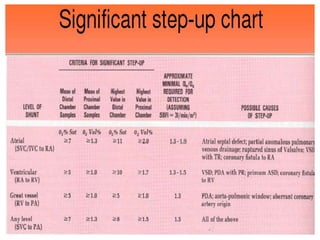
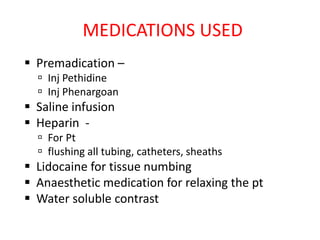
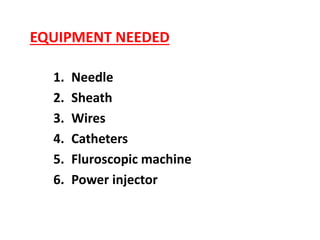
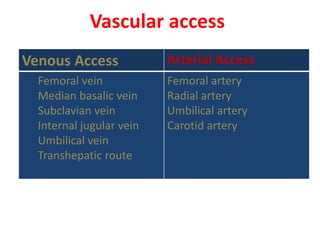
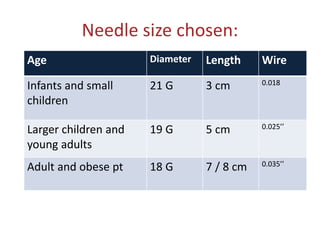
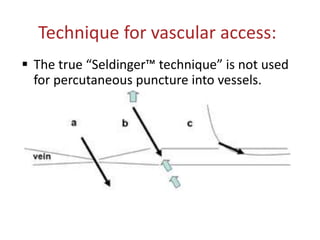
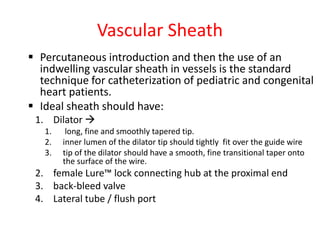
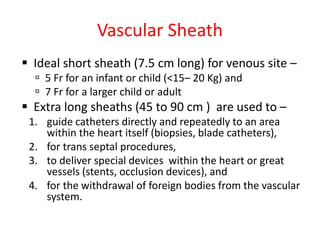
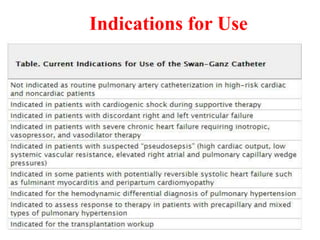
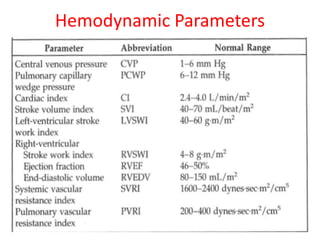
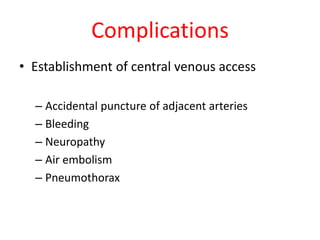
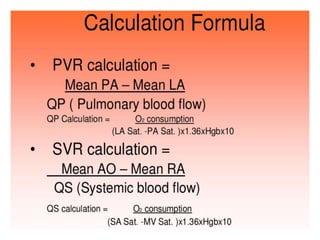
The document is a comprehensive overview of right heart catheterization (RHC), detailing its history, indications, contraindications, and classification of diagnostic and therapeutic purposes. It covers the technical aspects, equipment needed, vascular access techniques, and hemodynamic parameters monitored during the procedure. Additionally, it addresses practice guidelines and possible complications associated with pulmonary artery catheterization.