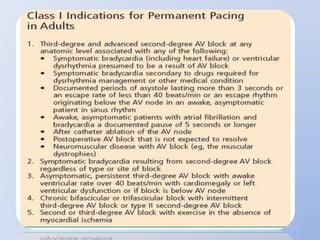
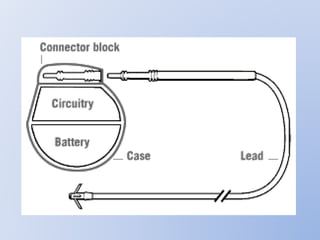
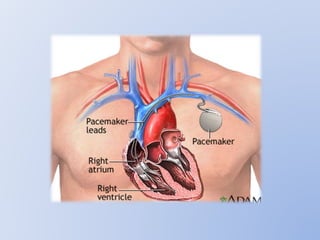
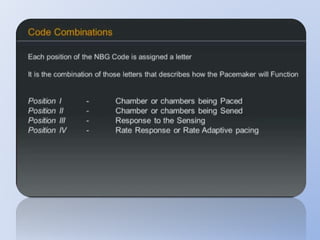
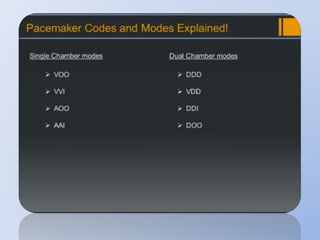
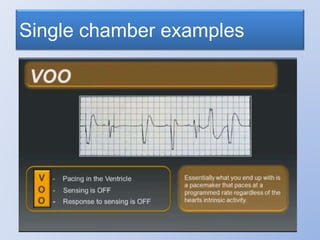
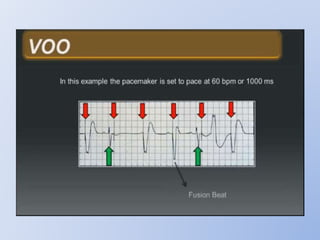
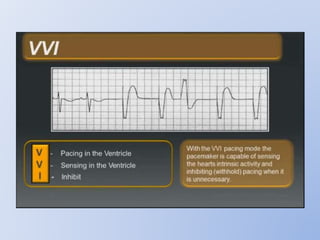
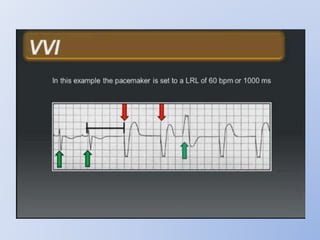
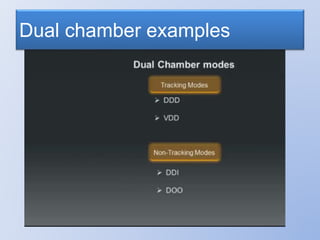
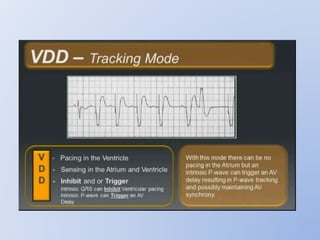
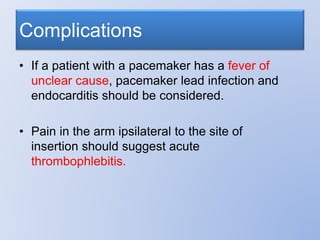
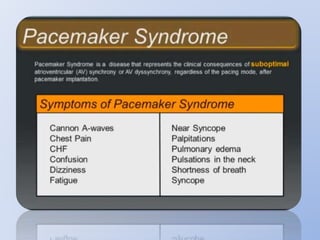
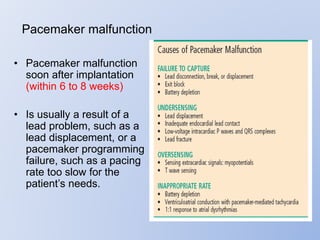
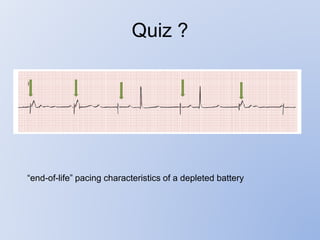
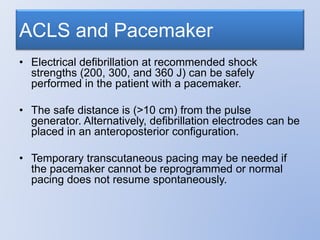
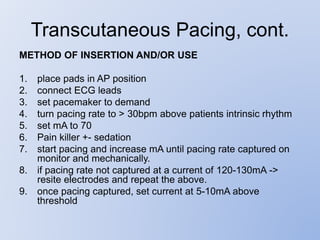
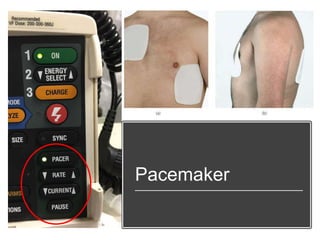
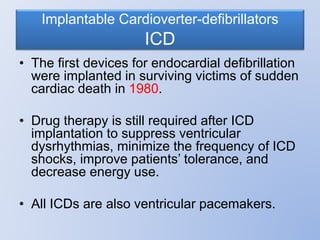
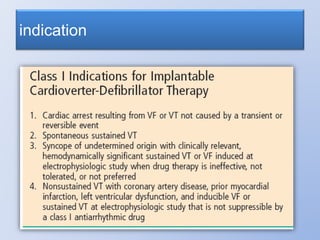
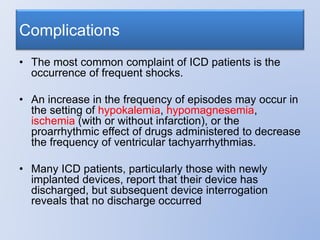
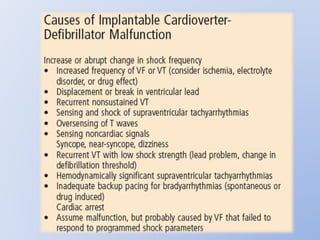
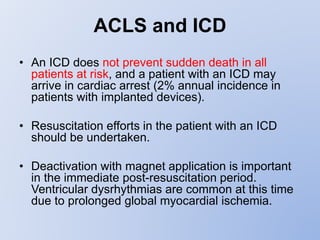
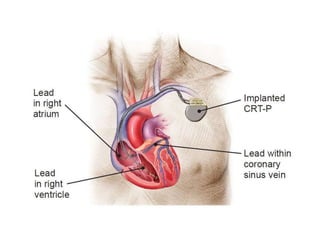
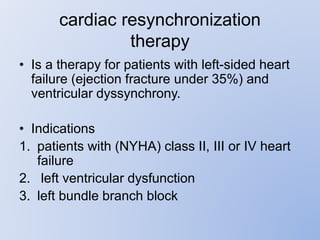
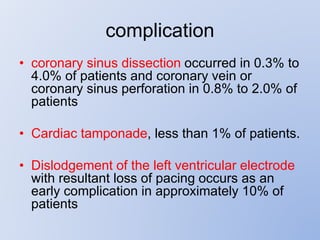
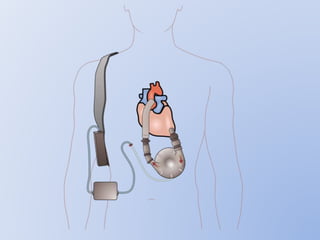
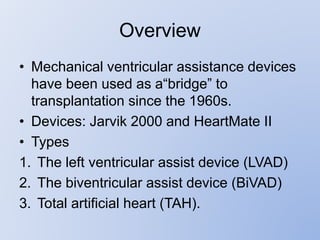
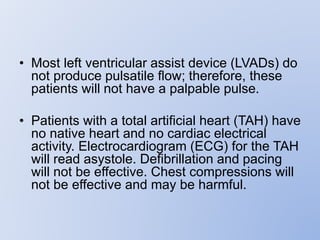
This document discusses various implantable cardiac devices including pacemakers, implantable cardioverter-defibrillators (ICDs), cardiac resynchronization therapy (CRT), and cardiac assist devices. It describes the components, indications, and complications of pacemakers and ICDs. It also covers topics such as pacemaker/ICD terminology, programming, interactions with defibrillation, and transcutaneous pacing. Cardiac assist devices are briefly discussed, noting examples like LVADs, BiVADs, and total artificial hearts.