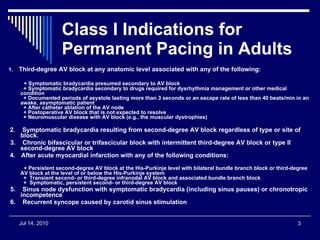
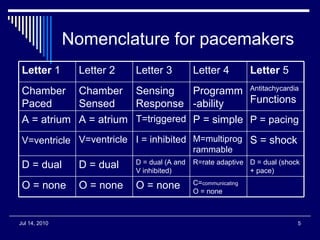
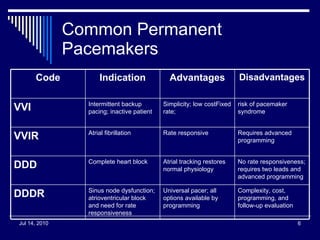
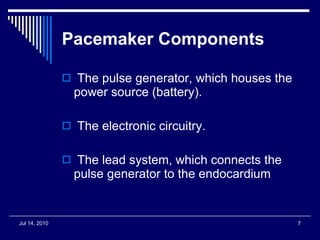
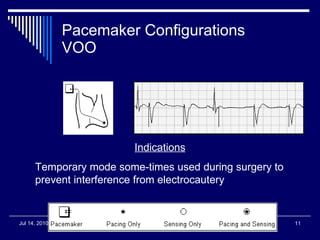
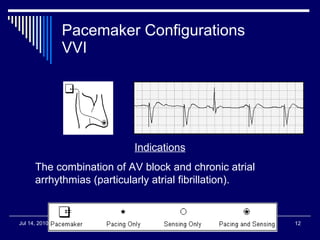
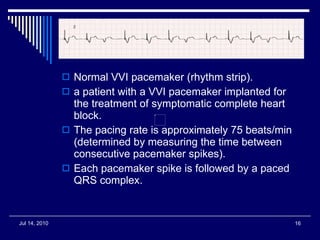
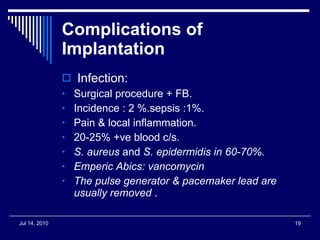
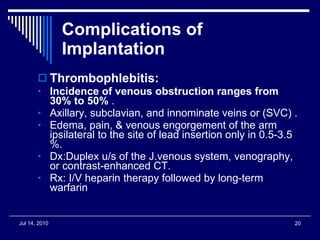
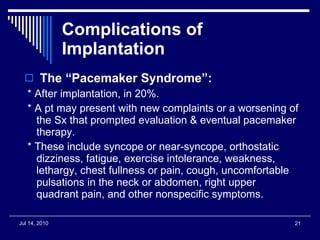
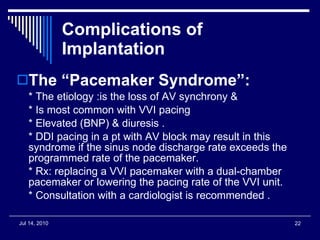
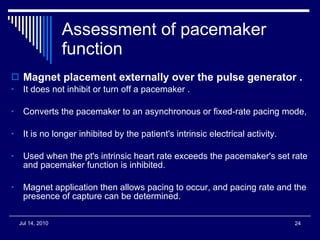
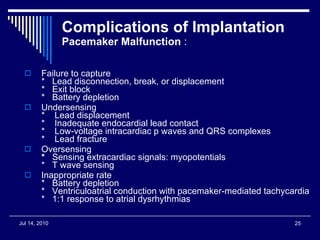
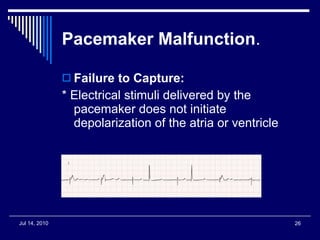
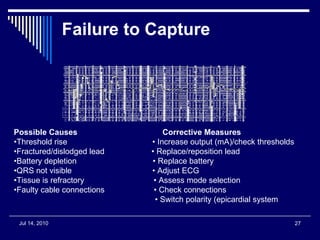
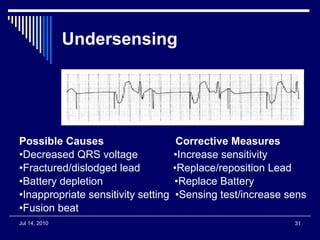
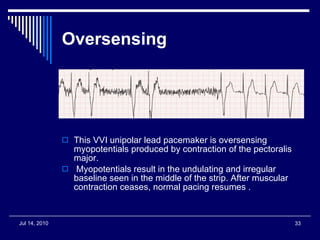
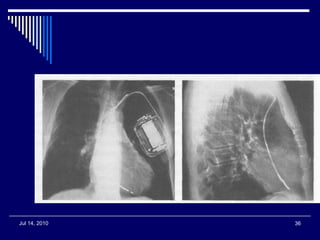
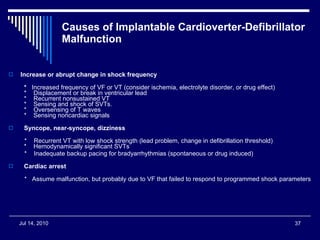
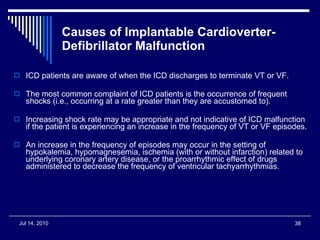
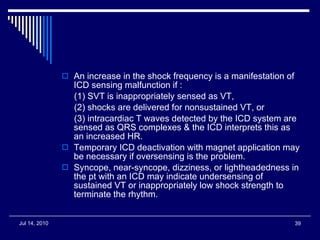
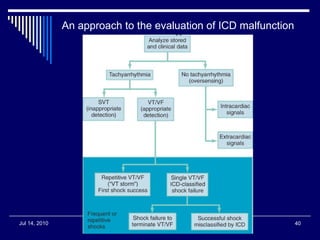
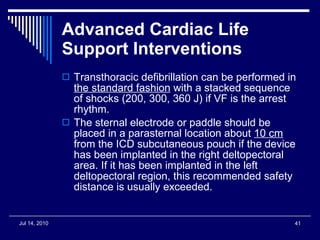
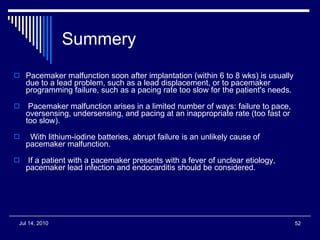
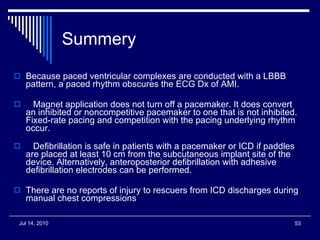
This document provides an overview of pacemakers and implantable cardioverter-defibrillators (ICDs), including indications, components, configurations, complications, and management. It discusses pacemaker and ICD malfunctions such as failure to pace or sense appropriately, inappropriate pacing rates, and increased shock frequencies. The document emphasizes that pacemaker/ICD malfunctions usually indicate lead problems or changes in the underlying cardiac condition, and stresses consulting cardiologists for device evaluation and potential reprogramming or reimplantation.