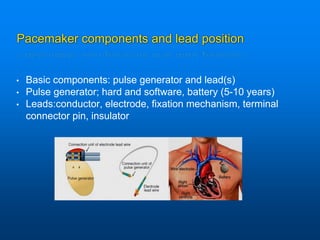
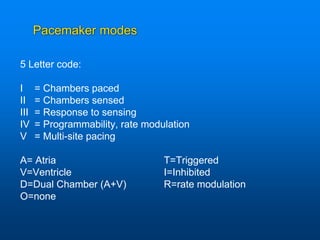
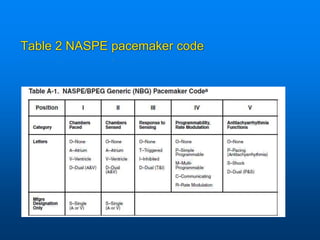
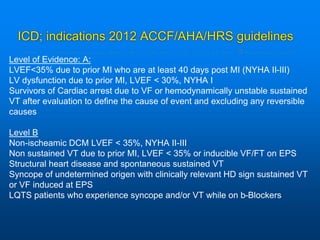
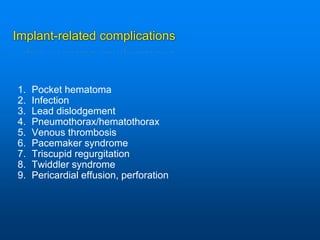
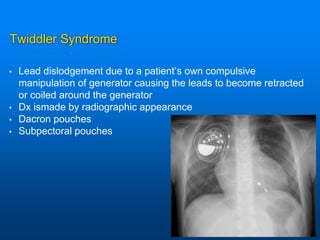
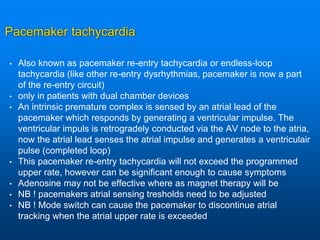
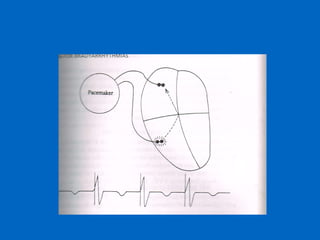
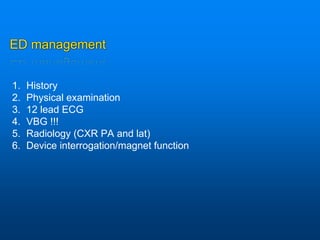
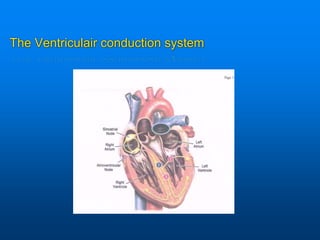
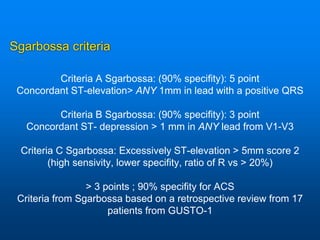
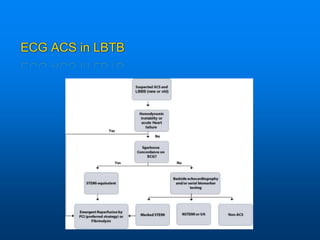
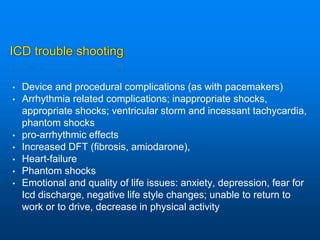
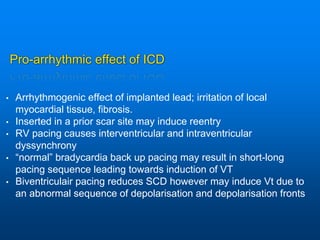
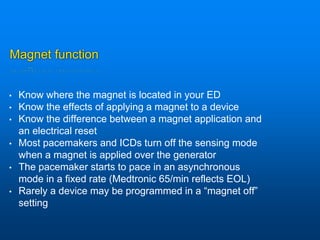
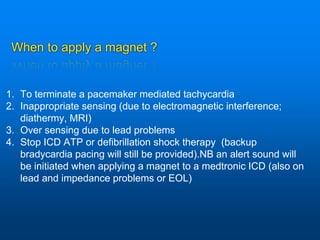
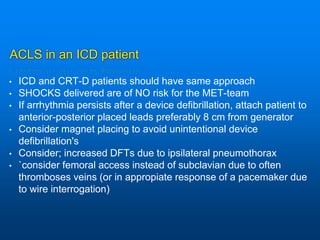
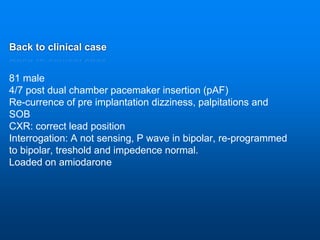
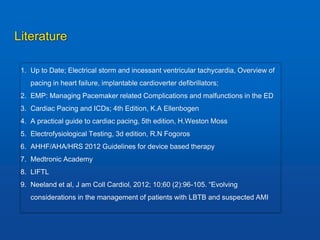
This document discusses emergency issues related to pacemakers and implantable cardioverter defibrillators (ICDs). It covers clinical cases, device components and functions, complications, and emergency department management strategies. Key points include descriptions of pacemaker modes and indications for pacemakers, cardiac resynchronization therapy, and ICDs. Common complications like infection, lead issues, and inappropriate shocks are reviewed. The document stresses the importance of obtaining a history, physical exam, ECG, and device interrogation in the ED. Magnet use and Sgarbossa criteria for diagnosing acute MI in paced patients are also summarized.