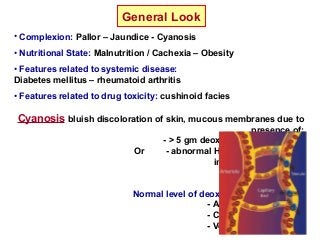
This document provides information on performing a clinical assessment of the respiratory system. It discusses obtaining a history, performing a general examination including vital signs and systemic review, and examining the chest. It describes point of care devices like glucometers and pulse oximeters. Investigation methods covered include respiratory function tests, chest x-rays, and ECGs. Common respiratory symptoms like dyspnea, cough, hemoptysis, and chest pain are defined. Examination findings and adventitious lung sounds are also outlined.