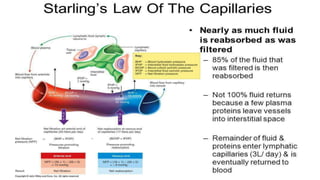
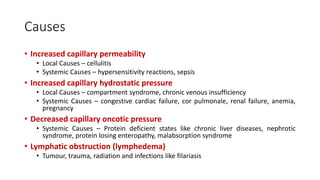
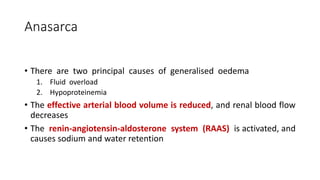
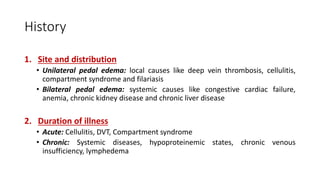
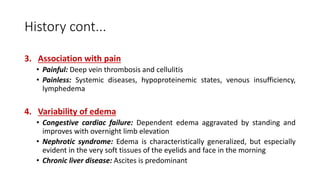
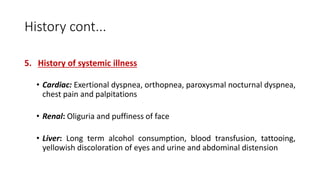
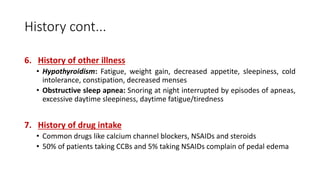
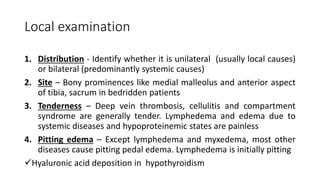
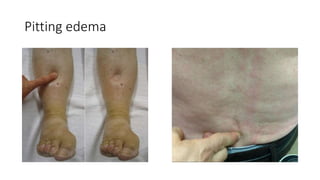
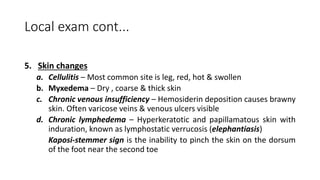
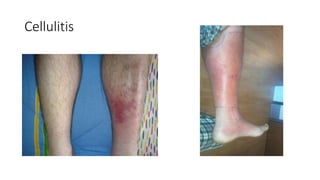
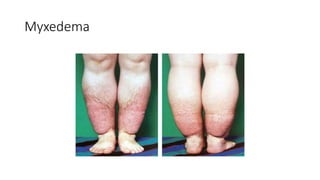
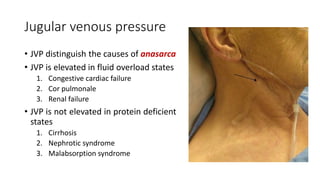
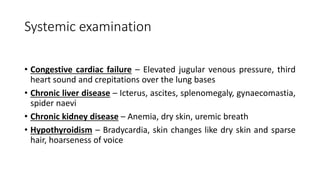
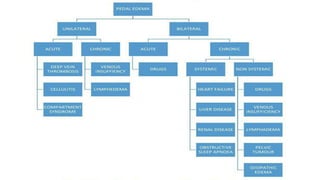
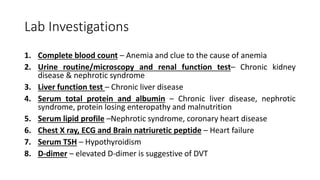
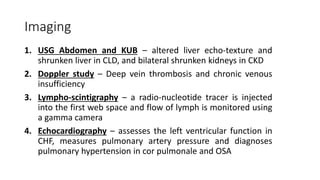
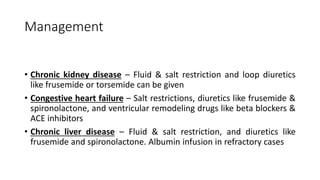
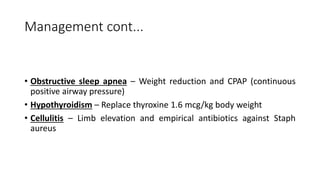
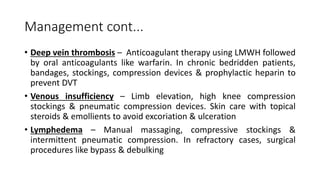
A 62-year-old man with bilateral pedal edema and shortness of breath was diagnosed with congestive heart failure after examination and investigations. The document discusses the causes, history, and management of edema, emphasizing the importance of clinical examination and various diagnostic tests. Management strategies for different underlying conditions include diuretics, lifestyle changes, and specific treatments based on the etiology of fluid retention.