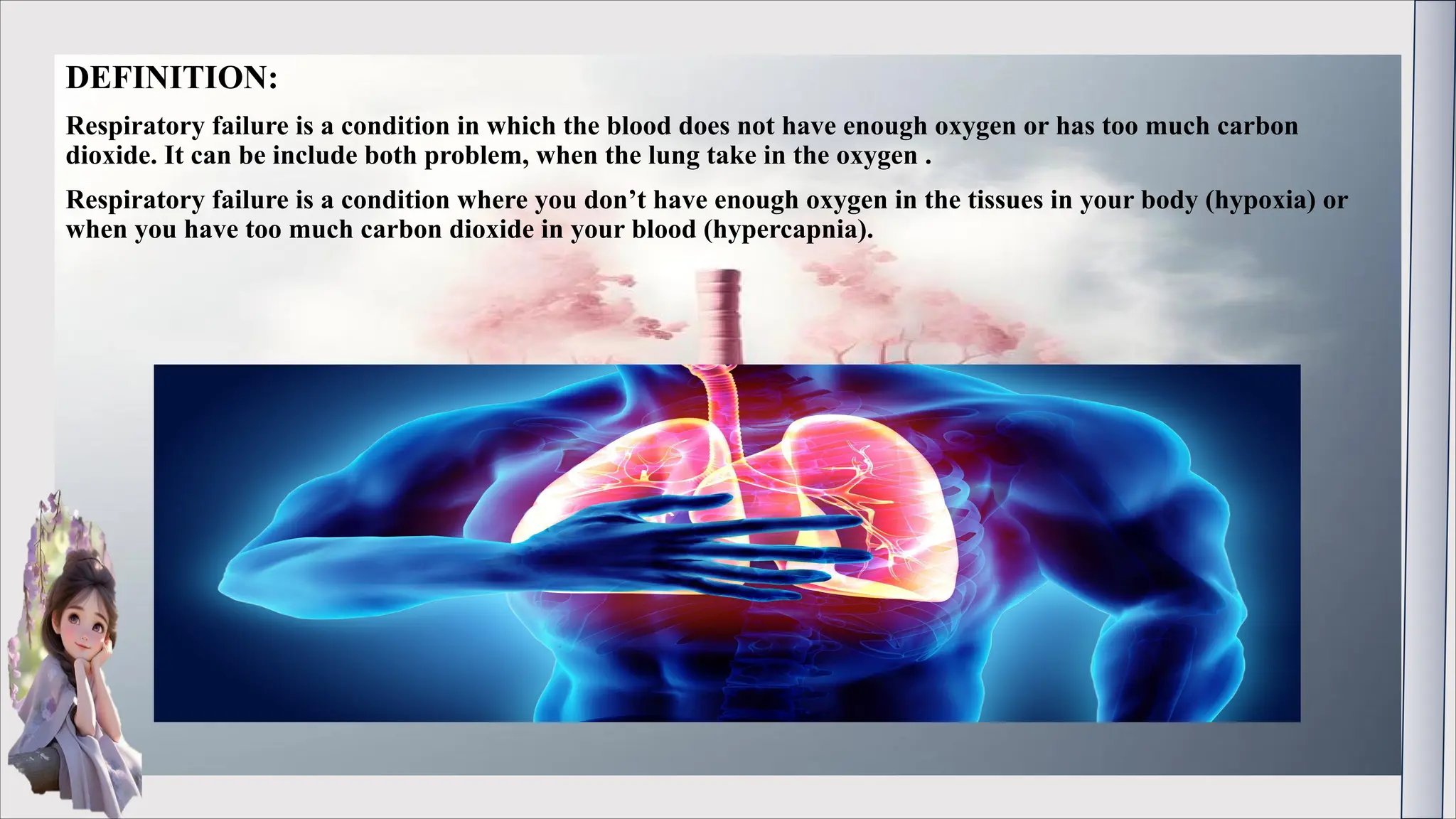
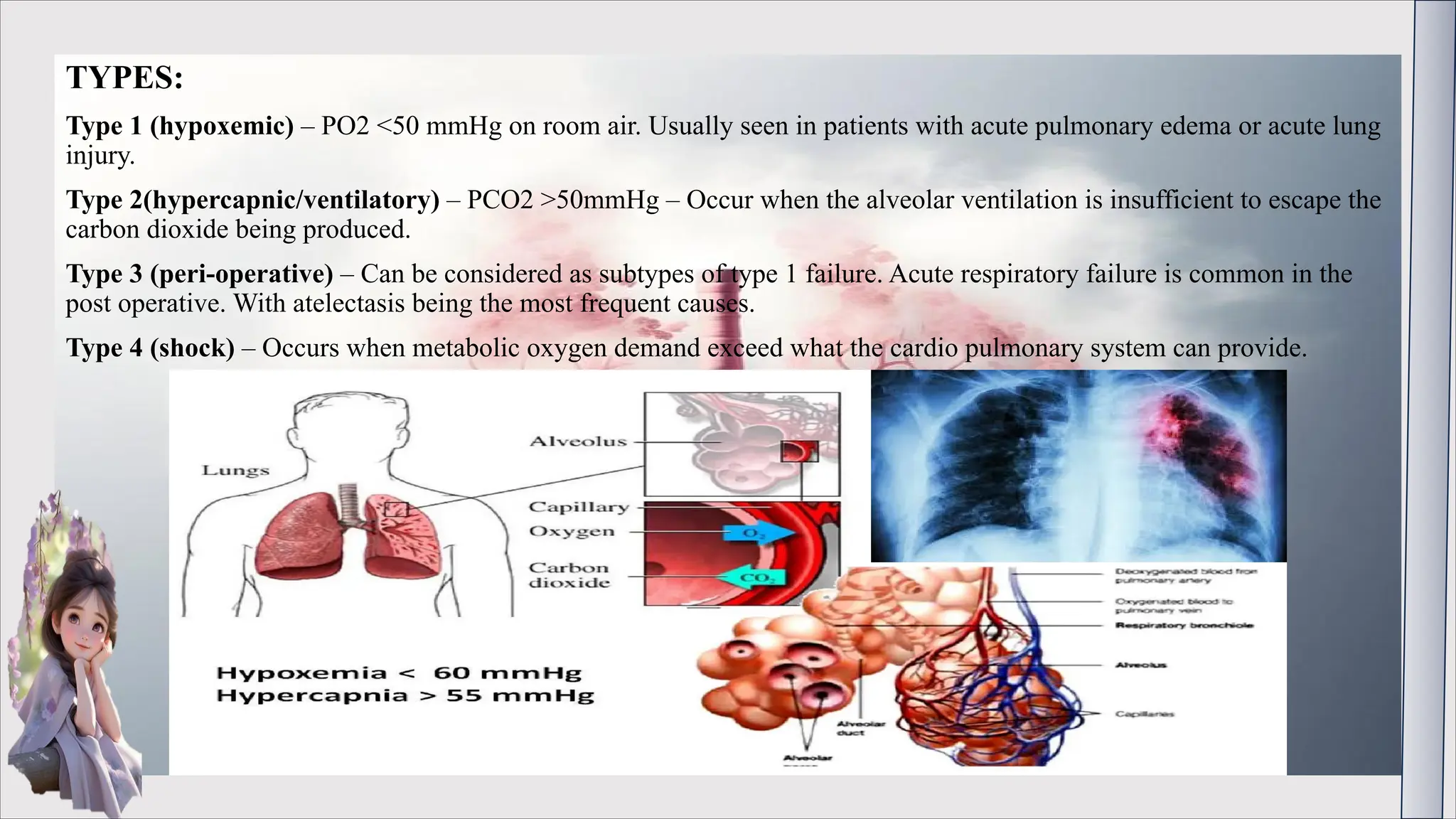
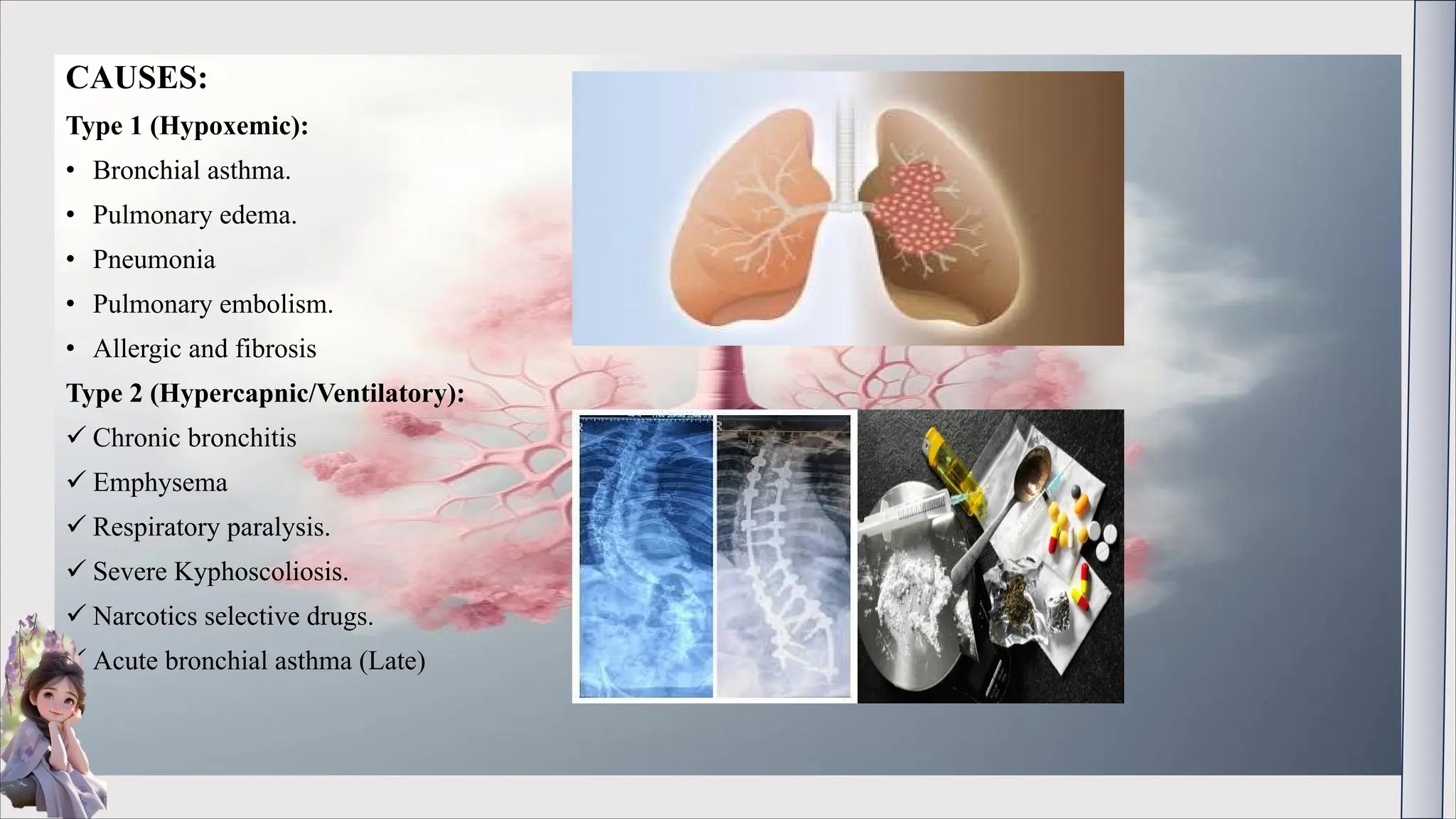
Respiratory failure is a condition characterized by inadequate oxygenation of the blood or excessive carbon dioxide, which can manifest as hypoxia or hypercapnia. It is classified into four types, each with specific causes and symptoms, including shortness of breath, rapid heartbeat, and cyanosis. Diagnosis involves various tests, and treatment options include mechanical ventilation, oxygen therapy, and managing underlying conditions.