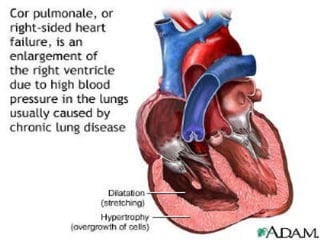
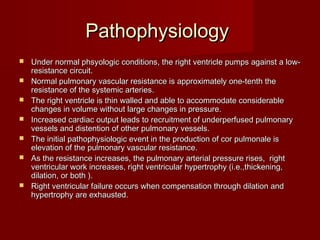
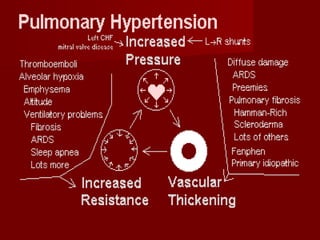
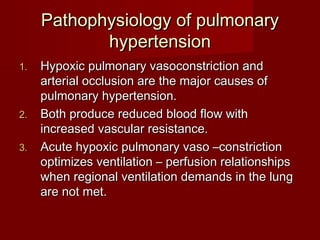
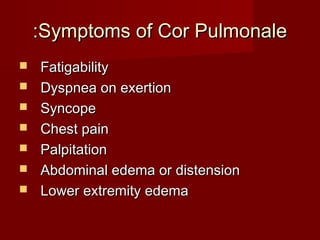
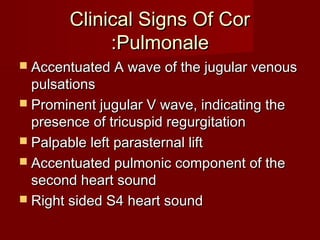
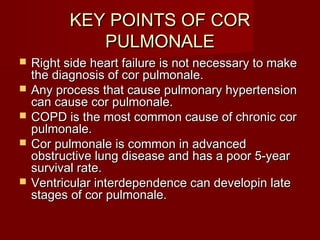
Cor pulmonale is a condition where the right ventricle of the heart enlarges and fails due to long-standing increased workload from diseases that affect the lungs like COPD. It is defined as hypertrophy and dilation of the right ventricle resulting from increased pulmonary vascular resistance. The main causes are chronic hypoxemia and pulmonary thromboembolism which lead to remodeling of the pulmonary arteries and increased pressure in the lungs. Over time, this puts strain on the right ventricle and can cause it to fail. Treatment focuses on reducing pulmonary pressures through oxygen therapy and vasodilators while managing symptoms of right heart failure.