1) Acute respiratory distress syndrome (ARDS) is a life-threatening lung condition caused by direct or indirect injury to the lungs whereby the alveolar capillary membrane becomes damaged and permeable, resulting in pulmonary edema.
2) ARDS is characterized by hypoxemia, reduced lung compliance, and diffuse pulmonary infiltrates seen on chest imaging.
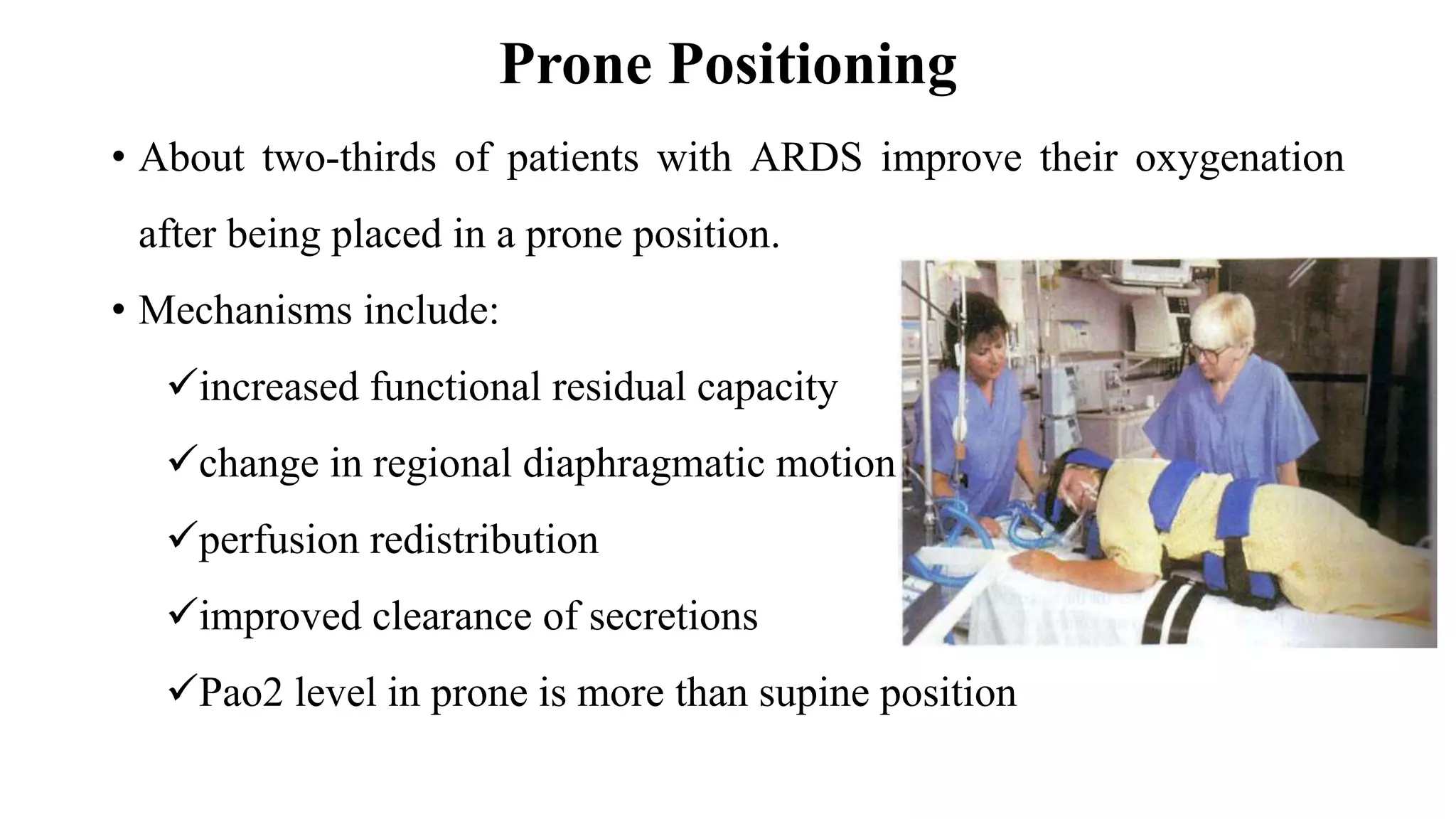
3) Treatment involves supportive care in an intensive care unit including mechanical ventilation, supplemental oxygen, and positioning therapies like prone positioning to improve oxygenation.