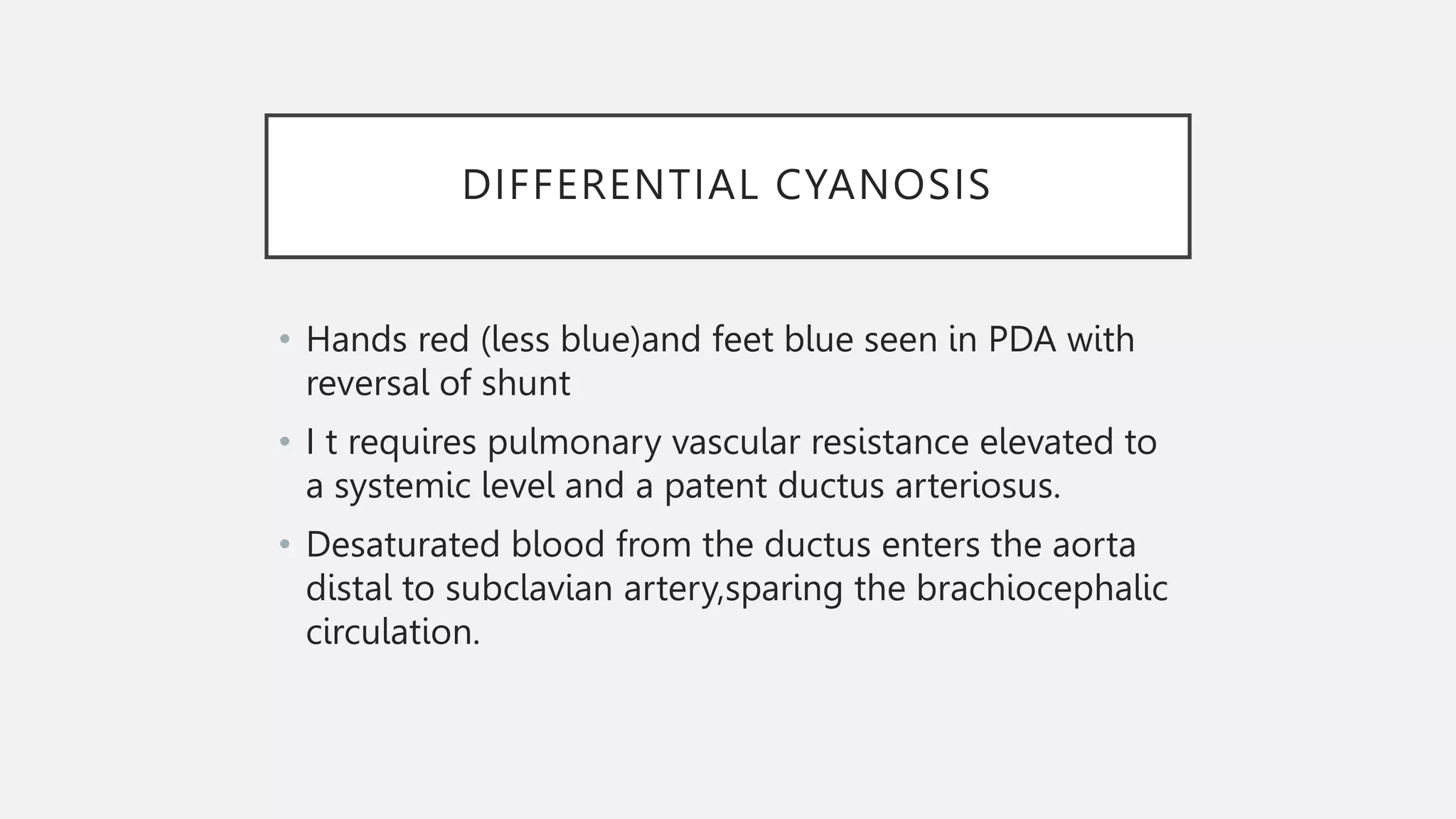
This document discusses cyanosis, defined as a bluish discoloration of the skin and mucous membranes due to low oxygen saturation in the blood. It describes two main types of cyanosis - peripheral and central cyanosis. Peripheral cyanosis is caused by low oxygen saturation at the venous end of capillaries and affects the extremities. Central cyanosis involves decreased oxygen saturation in arterial blood and affects more central areas. Causes, signs, and treatments are provided for each type. Investigations like pulse oximetry, blood gases, and hyperoxia testing are also summarized to differentiate between cardiac and pulmonary causes of cyanosis.